World Contraception Day (WCD) is on 26 September. This annual worldwide campaign seeks to increase awareness of contraceptive options so that women and their partners have greater informed choice and fewer unwanted pregnancies. The vision of WCD, to ensure that every pregnancy is wanted, remains elusive in many countries, as an estimated half of all pregnancies globally are unplanned. Around one-third to a half of Australian women experience an unintended pregnancy in their lifetime1 and up to a third of Australian women will undergo an abortion.2 Fifty per cent of women who present for abortion in Australia and New Zealand are using a method of contraception. Many are relying on user-dependent methods, such as condoms or the oral contraceptive pill.3 4 Unintended pregnancies that do not result in abortion may result in poorer pregnancy outcomes than those that have been planned, with a higher incidence of adverse birth outcomes5 and serious social and psychological consequences for women and their families.
Evidence for the superior efficacy of LARC
Long-acting reversible contraceptive methods (LARC), in particular, intrauterine contraception (IUC) and subdermal etonogestrel (ENG) implants, are significantly less likely to result in unintended pregnancy than short-acting user-dependent methods, such as the oral contraceptive pill.6 7 In a large cohort study, these methods were found to be 20 times less likely to result in unintended pregnancy, compared to combined hormonal methods (the pill, patch or ring)6 (Figure 1). In addition, immediate initiation of LARC after abortion has been shown to reduce the rate of repeat abortion.8 9 10 IUC (copper intrauterine devices and the levonorgestrel intrauterine system) and ENG implants provide ‘fit and forget’ contraception for three to ten years and have higher continuation rates than short-acting contraception. LARC are more cost-effective than the contraceptive pill, even at one year of use.11 Despite this, the uptake of LARC methods in Australia remains low compared to other developed countries, with only 11 per cent of women using them.12 13 In contrast, 24 per cent of reproductive-aged women in Sweden use a LARC method.14Although the progestogen-only injectable contraceptive, Depo Provera®, fits the definition of LARC, it is regarded as a second-tier option, due to its lower efficacy.15 A self-administered, subcutaneous formulation of depot-medroxyprogesterone acetate, Sayana Press®, is available in the US and Europe. Self-administration of this contraceptive enables women to be given a yearly supply, offering greater choice and more autonomy over their contraception.16 17
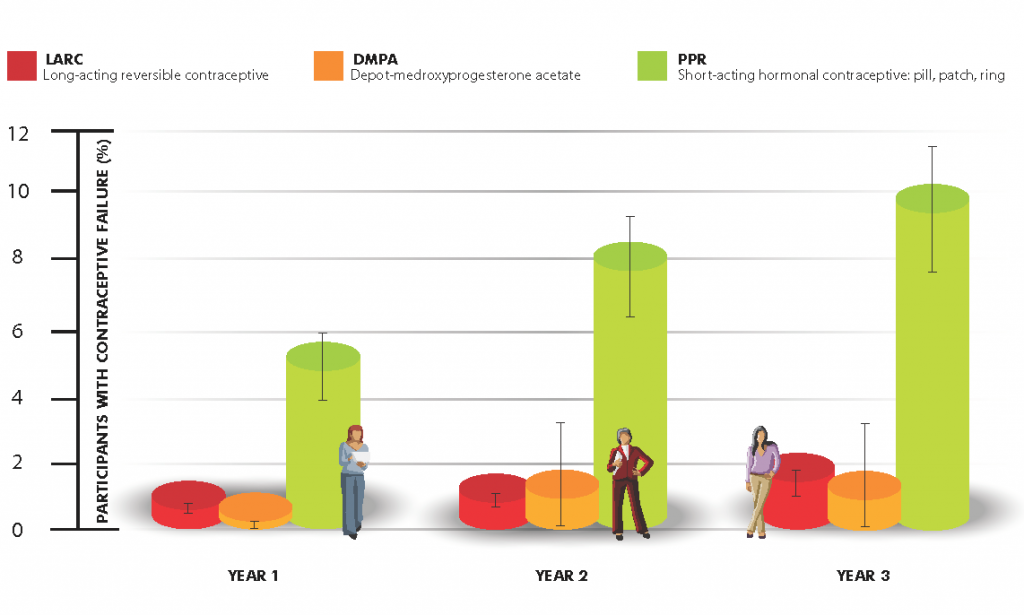
Figure 1. Comparison of unintended pregnancies by contraceptive method.
Recommendations for initiation of LARC
Historically, healthcare providers delayed commencement of a contraceptive method until the beginning of a normal menstrual period, to ensure there was no risk of pregnancy and that the method would become effective immediately. However, women present to their providers at different times of their menstrual cycle requesting contraception. Delaying initiation of her chosen method potentially exposes the woman to risk of an unintended pregnancy in the intervening time. This requirement for repeat visits adds an additional layer of complexity when, in many cases, taking a ‘quick start’ approach, initiating a contraceptive method at a time other than the start of the menstrual cycle will be safe and appropriate. In cases where pregnancy cannot be excluded, quick starting the levonorgestrel intrauterine system is not recommended and the copper intrauterine device should only be used if the criteria for its use as an emergency contraceptive are met.18
All LARC methods can be initiated immediately after surgical abortion. ENG implants can be inserted at the time of mifepristone administration for medical abortion and IUC can be inserted any time after expulsion of the pregnancy has been confirmed. Increasingly, women are choosing medical abortion or accessing services through telemedicine, with the procedure occurring at home, which makes early initiation of LARC more challenging. Women have high rates of non-attendance for a LARC interval insertion following abortion. In one study, only half of women fast-tracked to a contraceptive clinic after medical abortion actually attended, with the authors concluding that immediate insertion after medical abortion is preferable.19 If immediate insertion is not possible, greater likelihood of follow up is achieved if the appointment is scheduled within a few weeks of the abortion.20
Barriers to LARC
Knowledge and training
As advocates for women, healthcare professionals must ensure that women have access to a wide range of contraceptive options appropriate for their needs. A detailed understanding about the risks and benefits of LARC methods is paramount, both for contraceptive providers and consumers.21 Conveying the facts to women can be challenging, especially in light of recent adverse media coverage of LARC methods in Australia.22 Informing women of the advantages of LARC methods can be difficult, with research demonstrating that women’s knowledge regarding contraception is suboptimal and that misconceptions regarding side effects are common.23 24 Providing balanced information about the benefits of LARC, along with free provision, can result in as many as 70 per cent of women choosing IUC or an implant over other reversible methods6 and dispel misconceptions about their suitability.25
Provider-based barriers
Gaps in knowledge and training of LARC providers have been found to be a key barrier.26 A recent mixed methods study from the UK highlighted a number of issues, including a discordance between practitioner knowledge of eligibility for IUC and the medical eligibility criteria guidelines, lack of access to training, and risk aversion to undertaking procedures.26 Barriers among Australia primary care providers identified included a lack of: training in LARC insertion and removal, effective funding models for nurses to perform them, and availability of pathways for rapid referral.27 International research indicates a professional knowledge gap in familiarity with provision of IUC, with one of the major issues being misperceptions around the suitability of women for this method. Some providers are still reluctant to recommend or provide IUC methods for young or nulliparous women.23 24 25 This contradicts Australian and international evidence-based guidelines,28 29 which advocate the use of IUC in women of all ages and parity. Another barrier to accessing IUC may be the custom of mandating separate and multiple appointments for inserting devices.23 24 Many health services still initially offer a contraceptive counselling consultation and then request that the woman return at a later date for an insertion appointment. However, many women will be suitable for same-day insertion.
User barriers
There is a continued trend for young women to use short-term hormonal and barrier methods of contraception rather than LARC.16 17 A cross-sectional survey of more than 1500 men and women of reproductive age found that, despite the availability of highly effective methods of contraception in Australia, a considerable proportion of respondents used methods of low effectiveness, such as withdrawal and fertility awareness-based methods (FAMs).30 The increased use of FAMs may be associated with increased availability of smartphone applications, such as Clue and Kindara. Users of these methods should be aware that, with typical use, FAMs are only 76 per cent effective.31
The cost implications of LARC must also be considered in the Australian healthcare system. Removal of financial barriers has been shown to increase uptake of LARC in the United States.32
Overcoming barriers
-
Developing national standards and guidance
Scotland’s first National Sexual Health and Relationships Strategy, Respect and Responsibility: Scotland’s Strategy and Action Plan For Improving Sexual Health,33 was launched in 2005 with £15 million of funding over three years. This funding was extended by the Scottish government within the Better Health, Better Care: Action Plan.34 A range of actions were set out in this strategy to enhance sexual health promotion, education and service provision. National Health Service Quality Improvement Scotland (NHS QIS) developed clinical sexual health standards for services provided by, or secured by, NHS Scotland. NHS QIS also set standards for measuring the uptake of LARC methods and targets for increasing their use.36 was accepted by sexual health staff as having relevance to Scotland, as its findings addressed the same contraceptive issues that affected women and professionals in Scotland.
-
Empowering clinicians to address barriers
The NHS QIS standards and guidelines empowered clinicians to consider novel ways of overcoming barriers to LARC provision. One simple strategy employed in many settings in Scotland was to abolish the necessity for a pre-LARC fitting consultation. This reduced the time and inconvenience experienced by women and providers associated with multiple appointments, and lessened the risk of an unplanned pregnancy in the period between consultations. LARC fitting at the initial appointment is now available at a range of sexual and reproductive services in Scotland. This approach is also recommended in the United States.37 38 Other innovative approaches were the introduction of pre-appointment telephone consultations39 and the use of information DVDs viewed by women prior to their appointment.40 However, in many general practice settings, same-day LARC provision remains a challenge, due to time constraints and the need for advance prescriptions.26 Some general practices have overcome this obstacle by storing small supplies of LARCs, which are replenished as required.
-
LARC provision after pregnancy
There has been a strong focus on the provision of LARC in the abortion setting in Scotland, in line with NHS QIS standards41 and Faculty of Sexual and Reproductive Health guidelines.42 Doctors and nurses providing abortion care in Scotland have been trained to provide LARC methods. Access to immediate postnatal provision of subdermal implants has also been a focus of intervention, based on concern about the adverse impact of short inter-pregnancy intervals on perinatal outcomes.43 44 IUC is offered at the time of elective caesarean section.45 The Access to Post Partum Contraception in Edinburgh South East (APPLES) project is an example of a collaborative approach to postpartum contraceptive provision, where midwives were trained and identified as ‘contraceptive champions’, able to insert implants, as well as administer Depo Provera.46 A home ENG implant insertion service was also introduced for vulnerable women, in recognition of the fact that immediate postpartum provision is not always possible.47 If maternity services are to be engaged in providing quality postpartum contraception, it is crucial that midwives and other members of the multidisciplinary team are provided with training and support to offer this service. Contraceptive ENG implant training for midwives has added enormous capacity to the system and ensures that better use is made of the valuable resources,48 although time pressures and adequate knowledge remain ongoing challenges.49
Table 1. Summary of LARC methods: components, duration, efficacy and absolute contraindications.50
Method |
Trade name |
Active ingredient |
Duration of action |
Efficacy |
Absolute contraindications |
| ENG implant | Implanon NXT | The single rod (4cm) implant contains 68mg of the progestogen etonogestrel | 3 years | 99.95% | Breast cancer |
| LNG implant | Jadelle (available in NZ) |
2 rods, each containing 75mg levonorgestrel | 5 years | 99.95% | Breast cancer |
| Copper-IUD | TT380 Standard
TT380 short Load-Cu 375 |
Copper surface area from 375–380mm2 | 5–10 years | 99.2% | Unexplained vaginal bleeding, puerperal sepsis, GTD* (persistently elevated BHCG levels or malignant disease), current PID#, symptomatic untreated STIs, reproductive tract tumours |
| LNG-IUS | Mirena | Levonorgestrel 52mg | 5 years | 99.8% | Unexplained vaginal bleeding, breast cancer, postpartum or postabortal sepsis, GTD (persistently elevated BHCG levels or malignant disease), current PID, symptomatic untreated STIs, reproductive tract tumours |
RANZCOG initiative in increasing LARC uptake
-
Development of training modules and guidance
RANZCOG’s special interest group in sexual and reproductive health has developed online modules in LARC. The training package contains three modules:
• Introduction to LARC
• Introduction to IUC insertion
• Insertion and management of IUC.These modules are available to RANZCOG members through Climate and free to non-RANZCOG members through the shop portal. These modules provide theory and clinical guidance for IUC methods.Implant training is no longer being provided by the pharmaceutical company. They have, however, been instrumental in the development of a guidance document: The safe and effective insertion and removal of Implanon NXT by health care professionals in Australia. The document, which has been endorsed by the Family Planning Alliance, includes competencies and examples of learning outcomes for implant insertion. -
Development of a pathway for training in sexual and reproductive health
RANZCOG has developed an Advanced Training Module (ATM) in contraception and abortion care and a sexual health online module. These modules will enable trainees to develop high-level skills and be able to provide clinical leadership.
Ongoing challenges
Ensuring adequate training of general practitioners remains a challenge, particularly for IUC. Increasingly, hospitals are not providing contraceptive services and the community training opportunities in state-based family planning clinics are limited. New models of care are being considered, such as a hub and spoke design, whereby hospitals and some GP practices are identified as centres of excellence and develop recognition as training centres.
References
- Rowe H, Holton S, Kirkman M, et al. Prevalence and distribution of unintended pregnancy: the Understanding Fertility Management in Australia National Survey. Aust N Z J Public Health 2016;40:104-9.
- Scheil W, Jolly K, Scott J, et al. Pregnancy Outcome in South Australia 2015. In: Health S, ed. Adelaide: Government of South Australia; 2015.
- Real choices: women, contraception and unplanned pregnancy. Marie Stopes International Australia, 2008. Available at: www.mariestopes.org.au/research/australia/.
- Weisberg E, Goldstone P, Heckenberg M. A profile of women terminating pregnancies in NS. First National Sexual & Reproductive Health Conference. Melbourne: Public Health Association Australia; 2012.
- Gipson J, Koenig M, Hindin M, et al. The effects of unintended pregnancy on infant, child, and parental health: a review of the literature. Studies in Family Planning 2008;39:18-38.
- Winner B, Peipert J, Zhao Q, et al. Effectiveness of long-acting reversible contraception. New England Journal of Medicine; 366:1998-2007.
- Birgisson N, Zhao Q, Secura G, et al. Preventing unintended pregnancy: the Contraceptive CHOICE Project in review. Journal of Women’s Health 2015;24:349-53.
- Cameron S, Glasier A, Chen Z, et al. Effect of contraception provided at termination of pregnancy and incidence of subsequent termination of pregnancy. BJOG 2012;119:1074-80.
- Heikinheimo O, Gissler M, Suhonen S. Age, parity, history of abortion and contraceptive choices affect the risk of repeat abortion. Contraception 2008;78:149-54.
- Roberts H, Silva M, Xu S. Post abortion contraception and its effect on repeat abortions in Auckland, New Zealand. Contraception 2010;82:260-5.
- Mavranezouli I. The cost-effectiveness of long-acting reversible contraceptive methods in the UK: Analysis based on a decision-analytic model developed for a National Institute for Health and Clinical Excellence (NICE) clinical practice guideline. Human Reproduction 2008;23:1338-45.
- Richters J, Fitzadam S, Yeung A, et al. Contraceptive practices among women: the second Australian study of health and relationships. Contraception 2016;94:548-55.
- Mazza D, Harrison C, Taft A, et al. Current contraceptive management in Australian general practice: an analysis of BEACH data. Medical Journal of Australia 2012;197:110-4.
- Kopp Kallner H, Thunell L, Brynhildsen J, et al. Use of contraception and attitudes towards contraceptive use in Swedish women – a nationwide survey. PLoS One 2015; 10:e0125990.
- Trussell J. Contraceptive failure in the United States. Contraception 2011;83:397-404.
- Cameron S. Subcutaneous depo-medroxyprogesterone acetate. Journal of Family Planning and Reproductive Health Care 2013; 39:75-7.
- Cameron S, Glasier A, Johnstone A. Pilot study of home self-administration of subcutaneous depo-medroxyprogesterone acetate for contraception. Contraception 2012;85:458-64.
- Faculty of Family Planning and Reproductive Health Care. FFPRHC Guidance: Quick Starting Contraception London: FSRH; 2017.
- Cameron S, Berugoda N, Johnstone A, Glasier A. Assessment of a ‘fast-track’ referral service for intrauterine contraception following early medical abortion. J Fam Plann Reprod Health Care 2012;38:175-8.
- Saav I, Stephansson O, Gemzell-Danielsson K. Early versus delayed insertion of intrauterine contraception after medical abortion – a randomized controlled trial. PLoS One 2012; 7:e48948.
- NHS Health Scotland. Awareness and knowledge of long acting reversible contraception: what women and professionals in Scotland need. Feedback from Qualitative Research. Edinburgh: NHS Health Scotland; 2009.
- Branley A. Spotlight on Implanon and Mirena long-acting reversible contraceptives, as women report severe side-effects Sydney: ABC News; 2017.
- Glasier A, Scorer J, Bigrigg A. Attitudes of women in Scotland to contraception: a qualitative study to explore the acceptability of long-acting methods. Journal of Family Planning & Reproductive Health Care 2008;34:213-7.
- Bateson D, Harvey C, Williams J, Black K. Intrauterine contraception: why are so few Australian women using this effective method? Medical Journal of Australia 2011;194(6):324.
- Walker S, Newton V, Hoggart L, Parker M. ‘I think maybe 10 years seems a bit long.’ Beliefs and attitudes of women who had never used intrauterine contraception. BMJ Sexual & Reproductive Health 2018;44:90-6.
- Hoggart L, Walker S, Newton V, Parker M. Provider-based barriers to provision of intrauterine contraception in general practice. BMJ Sexual & Reproductive Health 2018;44:82-9.
- Mazza D, Bateson D, Frearson M, et al. Current barriers and potential strategies to increase the use of long-acting reversible contraception (LARC) to reduce the rate of unintended pregnancies in Australia: An expert roundtable discussion. ANZJOG 2017;57:206-12.
- Family PLanning NSW, Family PLanning Victoria, Health. TRaR. Contraception: an Australian clinical practice handbook, 4th edition. Ashfield, NSW 2014.
- Intrauterine Contraception. FSRH, 2015.
- Freilich K, Holton S, Rowe H, et al. Sociodemographic characteristics associated with the use of effective and less effective contraceptive methods: findings from the Understanding Fertility Management in Contemporary Australia survey. European Journal of Contraception & Reproductive Health Care 2017;22:212-21.
- Fertility Awareness Methods. FSRH, 2015.
- Secura G, Allsworth J, Madden T, et al. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. American Journal of Obstetrics and Gynecology 2010;203:115.e1-.e7.
- The Scottish Executive Health Department. Respect and responsibility. Strategy and action plan for improving sexual health. In: Department TSEH, ed. Edinburgh 2005.
- Scotland N. Better Health, Better Care: Action Plan. In: Scotland H, ed. Edinburgh: The Scottish Government; 2007.
- Standards for sexual health services. Healthcare Improvement Scotland, 2008. Available on pdf via: www.healthcareimprovementscotland.org/previous_resources/standards/sexual_health_services_final_s.aspx./note] Objectives for effective contraception after abortion were included in these standards. Additionally, the 2005 National Institute for Health and Clinical Effectiveness (NICE) guidance on the use of LARC35National Institute for Clinical Evidence. Long-acting reversible contraception. 2005.
- ACOG Committee. Increasing use of contraceptive implants and intrauterine devices to reduce unintended pregnancy. Obstetrics & Gynecology 2009;114:1434-8.
- Biggs M, Arons A, Turner R, Brindis C. Same-day LARC insertion attitudes and practices. Contraception 2013;88:629-35.
- Gorman C, Dennis J, Heathcote J. Telephone counselling for subdermal implants and intrauterine contraceptives. BMJ Sex Reprod Health 2018;44:136-8.
- Gunn C, Gebbie A, Cameron S. ‘One-stop’ visits for insertion of intrauterine contraception using online resources. J Fam Plann Reprod Health Care 2015;41:300-2.
- Standards for sexual health services. Healthcare Improvement Scotland, 2008. Available on pdf via: www.healthcareimprovementscotland.org/previous_resources/standards/sexual_health_services_final_s.aspx.
- FSRH Guideline Contraception After Pregnancy. FSRH, 2017.
- Heller R, Cameron S, Briggs R, et al. Postpartum contraception: a missed opportunity to prevent unintended pregnancy and short inter-pregnancy intervals. J Fam Plan Reprod Health Care 2016; 42:93-8.
- Health Promoting Health Service. NHS Scotland. Long-Acting Reversible Contraception in antenatal and postnatal care. Case Study number 8, 2013. Available at: www.healthscotland.com/uploads/documents/21436-HPHSCaseStudy8LongActingReversibleContraception.pdf.
- Heller R, Johnstone A, Cameron S. Routine provision of intrauterine contraception at elective cesarean section in a national public health service: a service evaluation. Acta Obstet Gynecol Scand 2017;96:1144-51.
- Cameron S, Craig A, Sim J, et al. Feasibility and acceptability of introducing routine antenatal contraceptive counselling and provision of contraception after delivery: the APPLES pilot evaluation. BJOG 2017;124:2009-15.
- Croan L, Craig A, Scott L, et al. Increasing access to contraceptive implants in the postnatal period via a home insertion service by community midwives. BMJ Sexual & Reproductive Health 2018;44:61-4.
- Britton A, Connolly A. Long-acting reversible methods of contraception: unified training. J Fam Plan Reprod Health Care 2014;40:80-1.
- McCance K, Cameron S. Midwives’ experiences and views of giving postpartum contraceptive advice and providing long-acting reversible contraception: a qualitative study. J Fam Plan Reprod Health Care 2014;40:177-83.
- Faculty of Family Planning and Reproductive Health Care. UKMEC Summary Table Hormonal and intrauterine contraception. London: FSRH; 2016.






Leave a Reply