Following publication of the Term Breech Trial in 20001 there has been a massive reduction in the incidence of vaginal breech birth. This has dramatically reduced staff exposure and familiarity with delivery techniques.
Vaginal breech births will inevitably continue; however, some will be carefully planned for, with maternal choice and informed consent, while others will still be unexpected. This will be due to precipitate delivery, failure of detection in the antenatal period, limited success rates with external cephalic version, intrauterine fetal death and patients with poor attendance or compliance with care. It is therefore vital that despite lack of experience, clinician skills continue to be maintained.
This article will deal with management of the unexpected singleton breech delivery.
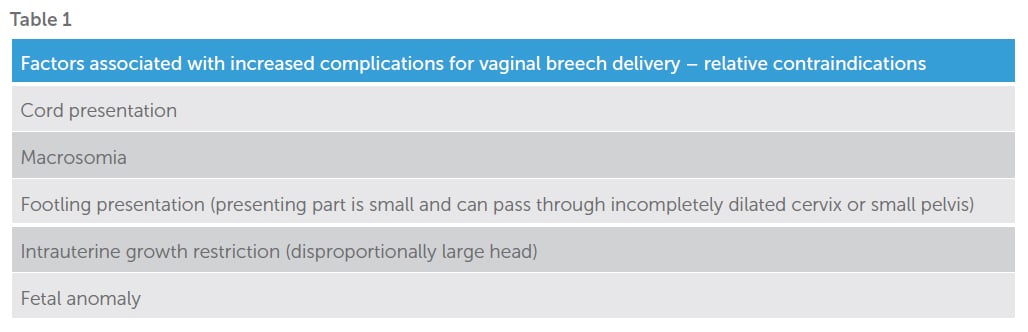
When a woman presents with an unexpected vaginal breech, management depends on the stage of labour, any factors associated with increased complications (Table 1), availability of clinical expertise and informed consent.2
An unexpected breech may present in labour or may be detected during a routine vaginal examination during labour or induction. At whatever point it is realised, a vaginal examination should be done to exclude cord presentation or prolapse, and ultrasound to estimate the position of the neck and legs.3
In a term pregnancy in early labour with no contraindications to vaginal delivery, the patient can be fully counselled toward maternal choice of trial of labour or caesarean section. There is a wide range of information available regarding how best to approach this.4 If there are contraindications, caesarean section should be encouraged.
Do not offer immediate caesarean section routinely if the patient presents in the second stage or in spontaneous premature labour up to 25+6 weeks gestation.5 6 A woman presenting in advanced labour and progressing well is likely to have an uncomplicated vaginal breech delivery.
If vaginal breech delivery is to go ahead, neonatal resuscitation equipment should be available. If diagnosed at home, an ambulance should be called for transfer to hospital.7
Delivery need not take place in an operating theatre, but ideally there should be recourse to a theatre and personnel, if needed. Emergency caesarean section may be required in 40 per cent of cases. Continuous electronic fetal monitoring (EFM) may lead to improved outcomes. A fetal scalp electrode can be attached to the buttocks if abdominal monitoring is difficult.8
There should be a low threshold for caesarean section with a breech in labour. Lack of progress in any stage or EFM signs of suspected fetal distress are good indications. Meconium liquor is not considered a sign of distress in a breech. Fetal blood sampling can be done from the buttocks. Membranes should be left intact, if possible, to reduce the risk of cord prolapse.
An epidural can be offered in view of the increased chance of intervention at delivery and to prevent involuntary pushing.9 Syntocinon is appropriate to promote passive descent for up to 90 minutes in the second stage and effective pushing.10 If delivery is not imminent after one hour of pushing, caesarean section should be performed. Total breech extraction is inappropriate for a term breech singleton.11 12 Delivery can occur on all fours, standing or semi-recumbent. Episiotomy can be done if needed, but not routinely. It should only be done once the fetal anus is visible on the perineum.13
If the woman has a strong urge to push, vaginal examination should be done to confirm full dilatation. Rectal dilatation may be noted as the fetal buttocks reach the ischial spines and perineal bulging below that. The fetus should not be touched until spontaneously delivered to the umbilicus, with shoulder blades visible. Complete delivery may then follow without any handling of the baby, save catching it!14
Risks at this point otherwise include nuchal arms and a trapped aftercoming head. Avoiding manipulation of the fetus as long as possible is thought to reduce both of these risks.
If spontaneous delivery does not progress, a towel can be wrapped around the fetal hips. Extended legs can be flexed by pressing behind the knees. This is the Pinard manoeuvre. 15 If the fetus is sacroposterior at this point it should be rotated to sacroanterior, and posterior rotation then prevented. Never hold the baby by the abdomen as this can easily rupture the fetal organs. Handling of the cord should be avoided. This causes vasospasm and reduction in flow.16
Lovsett’s manoeuvre can be used if the arms do not deliver spontaneously.17 The baby is held sacroanteriorly by its hips with thumbs on the sacrum. Lift and rotate 90 degrees to allow the posterior shoulder under the pelvic brim. Turn 180 degrees keeping the back anterior then dip downward and up for the anterior shoulder. If this fails to deliver the arms, pressure can be applied to the antecubital fossa until the wrist is accessible, then swept down. If this too fails, rotate the baby to sacroposterior facing upwards, which allows easier reaching of the antecubital fossae.

Figure 1. Delivery of fetal legs, step 1.

Figure 2. Delivery of fetal legs, step 2.
Once the arms are delivered, allow the baby to ‘hang’ at the perineum until the nape of the neck is visible. The head may spontaneously deliver with the next maternal effort.18 19If the head does not deliver easily and the fetus is premature, the cervix should be checked for full dilatation. If the cervix is felt trapping the head, it can be widened digitally, or Duhrssen incisions made – using scissors to cut the cervix at 2, 10 and 6 o’clock after administering tocolysis (usually terbutaline 0.25mg subcutaneously).20

Figure 3a. Lovsetts – Bony prominences.

3b. Lovsetts – First arm under pubic arch.

3c. Lovsetts – Fingers on upper arm.

3d. Lovsetts – Second arm.
If the head does not deliver easily, there are three options to encourage flexion:
- Burns-Marshall. The baby is held by the ankles and with ongoing maternal effort the trunk is directed in a wide arc from ‘hanging down’ to vertically upwards.21
- Suprapubic pressure can be used. This is the Bracht manoeuvre.22
- Mauriceau-Smellie-Veit manoeuvre. Support the baby on the one hand with legs over the arm. Put the other hand into the vagina, one finger on each of the fetal cheekbones and chin. Avoid traction on the jaw. Put the middle finger of the upper hand on the occiput to flex it, others either side on the shoulders.23
If repeated attempts of these manoeuvres do not deliver the head, Piper forceps can be used while an assistant holds the baby’s trunk and legs to 45 degrees above the horizontal.24 Insertion of blades can be very difficult and tocolysis may be needed. Blades should be brought together to sit below the fetal body. Literature reports suggest insertion of a Sims speculum to the posterior vaginal wall ‘to allow the baby a few breaths’, although if the head were low enough for this to actually occur it would likely be deliverable.25
Symphysiotomy is an uncommon manoeuvre that can be used at this point. Local anaesthetic should be infiltrated to the skin and down to the pubic symphysis. A rigid catheter should be inserted and used to displace the urethra laterally. Maternal legs should be abducted at 90 degrees. A scalpel should be used to cut down until the pubic symphysis separates enough for delivery. The incision can be sutured and the woman given crutches to mobilise after two days of bed rest.26

Figure 4a. Burns-Marshall, step 1.

4b. Burns-Marshall, step 2.

Figure 6. Allowing flexion of head.

Figure 7. Mauriceau-Smellie-Veit manoeuvre.
Last resort is the Zavanelli manoeuvre, pushing the fetus back into the maternal abdomen for emergency caesarean section. The majority of reports are related to caesarean section following shoulder dystocia.27 Morbidity and mortality rates for this procedure are unquantified. Tocolysis with maternal general anaesthesia is necessary for any chance of success.
All units should have a protocol for the arrival of a woman in advanced labour with a breech. As the situation is infrequent, simulation practice is recommended. This can be done by attending PROMPT, ALSO and/or InTime courses. In addition, a free video demonstrating manoeuvres can be found online at the WHO Reproductive Health Library.
For those faced with the situation in a location with no facilities, the main message would be to call for assistance and ‘keep your hands off the breech’.28 29 30
Photographs reproduced with permission from the PROMPT Maternity Foundation (Registered charity No:1140557): Original source from the PROMPT Course Manual (Second Edition) ISBN 9781107660526, August 2012, Cambridge University Press.
References
- Hannah ME, Hannah WJ, et al. Planned Caesarean section versus planned vaginal birth for breech presentation at term; a randomised multicentre trial. Lancet. 2000;356:1375.
- Kotaska A, Menticoglou S, Gagnon R. Vaginal delivery of breech presentation. J Obstet Gynaecol Canada. 2009;31(6)557.
- Womens and Newborn Health Service, King Edward Memorial Hospital Clinical Guidelines. Care of the unexpected breech. Department of Health Western Australia, 2015.
- Impey LWM, Murphy DJ, Griffiths M. RCOG Management of breech presentation BJOG. 2017. DOI:10.111/1471-0528./4465.
- Kotaska A, Menticoglou S, Gagnon R. Vaginal delivery of breech presentation. J Obstet Gynaecol Canada. 2009;31(6)557.
- Impey LWM, Murphy DJ, Griffiths M. RCOG Management of breech presentation BJOG. 2017. DOI:10.111/1471-0528./4465.
- Womens and Newborn Health Service, King Edward Memorial Hospital Clinical Guidelines. Care of the unexpected breech. Department of Health Western Australia, 2015.
- Impey LWM, Murphy DJ, Griffiths M. RCOG Management of breech presentation BJOG. 2017. DOI:10.111/1471-0528./4465.
- Womens and Newborn Health Service, King Edward Memorial Hospital Clinical Guidelines. Care of the unexpected breech. Department of Health Western Australia, 2015.
- Lewis P. Malpositions and malpresentations. In: Macdonald S, Magill-Cuerden J Editors. Mayes Midwifery 14th ed, Sydney, Balliere Tindall, 2011.
- Kotaska A, Menticoglou S, Gagnon R. Vaginal delivery of breech presentation. J Obstet Gynaecol Canada. 2009;31(6)557.
- Alarab M, Regan C, O’Connell MP. Singleton vaginal breech delivery at term; still a safe option? Obstetr Gynaecol. 2004;103:407.
- Kotaska A, Menticoglou S, Gagnon R. Vaginal delivery of breech presentation. J Obstet Gynaecol Canada. 2009;31(6)557.
- Impey LWM, Murphy DJ, Griffiths M. RCOG Management of breech presentation BJOG. 2017. DOI:10.111/1471-0528./4465.
- Alarab M, Regan C, O’Connell MP. Singleton vaginal breech delivery at term; still a safe option? Obstetr Gynaecol. 2004;103:407.
- Kotaska A, Menticoglou S, Gagnon R. Vaginal delivery of breech presentation. J Obstet Gynaecol Canada. 2009;31(6)557.
- Kotaska A, Menticoglou S, Gagnon R. Vaginal delivery of breech presentation. J Obstet Gynaecol Canada. 2009;31(6)557.
- Kotaska A, Menticoglou S, Gagnon R. Vaginal delivery of breech presentation. J Obstet Gynaecol Canada. 2009;31(6)557.
- Impey LWM, Murphy DJ, Griffiths M. RCOG Management of breech presentation BJOG. 2017. DOI:10.111/1471-0528./4465.
- Impey LWM, Murphy DJ, Griffiths M. RCOG Management of breech presentation BJOG. 2017. DOI:10.111/1471-0528./4465.
- Womens and Newborn Health Service, King Edward Memorial Hospital Clinical Guidelines. Care of the unexpected breech. Department of Health Western Australia, 2015.
- Alarab M, Regan C, O’Connell MP. Singleton vaginal breech delivery at term; still a safe option? Obstetr Gynaecol. 2004;103:407.
- Womens and Newborn Health Service, King Edward Memorial Hospital Clinical Guidelines. Care of the unexpected breech. Department of Health Western Australia, 2015.
- Kotaska A, Menticoglou S, Gagnon R. Vaginal delivery of breech presentation. J Obstet Gynaecol Canada. 2009;31(6)557.
- Alarab M, Regan C, O’Connell MP. Singleton vaginal breech delivery at term; still a safe option? Obstetr Gynaecol. 2004;103:407.
- Impey LWM, Murphy DJ, Griffiths M. RCOG Management of breech presentation BJOG. 2017. DOI:10.111/1471-0528./4465.
- Womens and Newborn Health Service, King Edward Memorial Hospital Clinical Guidelines. Care of the unexpected breech. Department of Health Western Australia, 2015.
- Womens and Newborn Health Service, King Edward Memorial Hospital Clinical Guidelines. Care of the unexpected breech. Department of Health Western Australia, 2015.
- Lewis P. Malpositions and malpresentations. In: Macdonald S, Magill-Cuerden J Editors. Mayes Midwifery 14th ed, Sydney, Balliere Tindall, 2011.
- Alarab M, Regan C, O’Connell MP. Singleton vaginal breech delivery at term; still a safe option? Obstetr Gynaecol. 2004;103:407.






Leave a Reply