General practitioner obstetricians (GPOs) provide the backbone to many rural and remote maternity services across Australia. They are involved in preconception care, antenatal, intrapartum and postpartum care, and provide care to the woman, her infant and family across the lifespan. They are in for the long haul.
The number of GPOs is in decline, due to factors including retirement of older doctors, maternity unit closures and substitution of GPO roles by midwives or junior doctors (Figure 1). We have been actively working to reverse this trend. In this article, we will discuss the importance of GPOs, consider barriers to GPO training, then share some ideas that we are using to bolster GPO training and retention in Western Australia.
Defining GP obstetrics and GPOs
For the purpose of this article, we define GPO as a GP who is involved not just in antepartum and postpartum care but also participates in the delivery of intrapartum care.1 In Australia and New Zealand, there are two levels of GPOs: those with a basic DRANZCOG, whose scope of practice includes non-complex deliveries more advanced gynaecological procedures, and those with an advanced DRANZCOG, whose scope of practice extends to complex deliveries, advanced gynaecological procedures and performance of basic early-and late- pregnancy ultrasound scanning.2
The current state of play
As of March 2021, there are 2070 basic diplomates and 561 advanced diplomates registered with RANZCOG; however, it is unknown how many are actually working to their full scope of practice. As a group, diplomates make up two-thirds of College membership.
Why we need GPOs
They provide holistic, integrated care of the woman and her family
GPOs are in the privileged position where they are able to provide not only obstetric but also medical and mental healthcare to women and their families. GPOs understand the individual, their family and their community, allowing them to provide unique, holistic support to the entire family unit.
They provide longitudinal continuity of care
As evidenced by the literature around midwifery continuity-of-care models, women value receiving their care from a known healthcare provider throughout their pregnancy, birth and postpartum, and their outcomes are improved as a result.3 4 GPOs often provide an extension of this longitudinal care, providing care from preconception to far beyond the six week postpartum check, ensuring that women and their baby receive true continuity of care.
They support maternity units close to where women live
It is well documented that women value being able to give birth close to home, particularly Aboriginal and Torres Strait Islander women.5 Maternity units supported by GPOs extend the range of services that can be provided on-site, ensuring that birthing women have access to effective analgesia, obstetric input during labour for more complex deliveries, and medical presence in the event of an obstetric emergency and/or neonatal resuscitation, optimising safety while maintaining access to local support networks.
They support their specialist obstetric and paediatric colleagues
This is particularly relevant to regional centres where there may only be one or two specialists covering the roster over a large geographical area. GPOs make up an integral part of the maternity team antenatally, intrapartum and postpartum, allowing sustainable rostering and service provision.
They provide general practice services to their communities
GPOs have a broad skill set in addition to maternity care. A single practitioner can concurrently provide essential general practice and emergency services in rural and remote locations.
So why is training GPOs so difficult?
Uncertainty about future job prospects
Lack of clear career pathways and exposure to negative stories of rural maternity unit closures or exclusion of GPOs results in anxiety about career prospects. Doctors in training require clear training pathways with viable job options upon completion, without having to relocate again and again.
Overlapping scope of practice with midwives
Unfortunately, there is a perception that GPO and midwifery care is competitive rather than complementary. In some instances, midwives may take over antenatal care to the exclusion of GPOs and liaise directly with their specialist obstetric colleagues when support is required. This results in a loss of access to holistic, integrated and continuity of care that GPOs can provide to women in collaboration with midwives.
Competition with specialist obstetric colleagues
Again, it is unfortunate that GPOs and specialists sometimes see one another as rivals rather than part of the same team. Some specialist obstetricians have concerns regarding standards of GPO practice, which leads to an unwillingness to back up their GPO colleagues. Further, some GPOs are hesitant to refer moderate-risk women to their specialist colleagues due to concerns that this may result in care being taken over unnecessarily, resulting in late requests for support that can compromise patient care. Mutual distrust is a significant barrier to providing woman-centred care.
Financial concerns
In order to be sustainable, GPO models of care must be financially viable. This is becoming increasingly difficult due to the competition that is arising between midwifery and specialist colleagues. On-call arrangements and salary versus fee-for-service models add complexity.
Lifestyle concerns
Many GPOs are now seeking positive work-life balance, which can be a challenge when juggling regular on-call services, family demands and their partner’s career. This can be compounded by lack of flexibility of maternity units to accommodate GPO’s unique needs.
High community expectation and litigation in obstetrics
Communities have expectations for obstetric care to be of a very high standard. When adverse obstetric outcomes occur, litigation is becoming more common. This is on a background of increased obstetric risk associated with higher rates of older women, obesity and assisted fertility (to name a few).
Fitting DRANZCOG training into GP training
GP registrars are required to demonstrate that they have performed sufficient diversity of skills during their training. GP registrars who complete their DRANZCOG training prior to commencing their GP training are under pressure to maintain their obstetrics skills while also acquiring new clinical skills during their GP training. This can be difficult to achieve and may lead to obstetric de-skilling.
Concerns regarding experience when newly qualified
With increasing competition for practical experience during hospital training, many newly graduated diplomates do not feel competent or confident to work autonomously as a GPO, particularly in rural towns with limited back up.
Feminisation of workforce and lack of re-skilling mechanisms
Rural Health West data indicates that the number of female GPOs is on the rise (Figure 1). Many newly qualified female GPOs take time off for their own maternity leave then need to regain confidence and skills when returning to clinical practice. Access to financially viable and family-friendly options for re-skilling are limited and can be a major barrier to GPOs returning to the workforce after a period of leave.
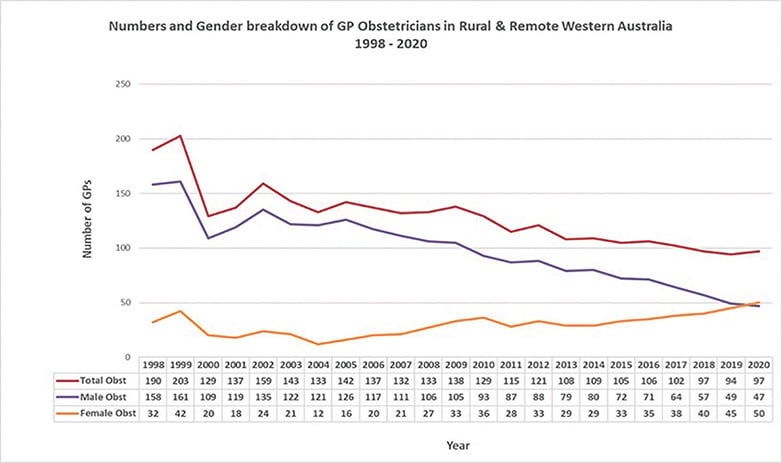
Figure 1. Numbers and gender breakdown of GPOs in rural and remote WA 1998–2020. * Peel Region GPs removed from the dataset from 2017 onwards due to changes in rural classification boundaries ** 2020 data is yet to be published and yet to be verified. Retrieved 26/3/2021 Source: Rural Health West Workforce Analysis Datasets 1998–2020
Credentialling issues
GPOs are increasingly scrutinised with regards to recency and frequency of experience in obstetrics skills when applying for hospital credentialing. These skills can be difficult to maintain in maternity units with smaller birth numbers and access to upskilling is limited.
The case for GPOs with basic and advanced DRANZCOG
There is a perception in some jurisdictions that all GPOs need to have advanced skills in order to provide the services required in regional and rural maternity units. We argue that there is also a place for basic diplomates for a number of important reasons. In small rural units, where rosters require GPOs to be on-call frequently, basic diplomates can be first on-call for non-complex obstetrics, allowing advanced diplomates to be second on-call for complex deliveries, which are less common. Further to this, basic diplomates can provide neonatal resuscitation in the event of complex deliveries. Finally, having a balance of basic and advanced diplomates ensures exposure to complex deliveries is not diluted and advanced diplomates have the opportunity to maintain these important skills.
How can we encourage and support GP obstetrics?
The continuation of GP obstetrics is predicated on a conviction that GPOs are an essential part of the delivery of obstetric care, particularly in regional, rural and remote Australia. For GP obstetrics to thrive, it needs the advocacy and support of its specialist O&G colleagues. O&G specialists must promote GP obstetrics as a career choice, actively participate in GPO training and upskilling, and work as supportive colleagues to GPOs.
There has been much discussion and indeed implementation of various strategies to encourage and support a career in GP obstetrics. These strategies need to be evaluated and successful strategies shared between jurisdictions. Funding for GPO training and support programs must be available, targeted and flexible.
Exposure of medical students and young doctors to successful models of GP obstetric care and inspiring GPOs is key to planting the idea of a career as a GPO. Once trained, measures to build confidence and competence and maintain skills are required. With the feminisation of the GPO workforce, and time taken off for family, reskilling programs are vital to retain female GPOs in this career.
The following are examples of initiatives undertaken in WA to encourage GP obstetrics and support GP obstetricians in WA
GP Obstetric Western Australian Advisory Group (GPOWAAG)
This group was created in 2007 to oversee the GPO mentoring program. The program provides funding and individualised support to newly qualified GPOs by nominated experienced GPO mentors in the first six to 12 months of GPO life. Evaluation of this program indicates success in building confidence and competence. There have been high rates of retention of GPOs in towns where they undertake their training and mentorship. GPOWAAG has also strengthened communication and relationships between the many stakeholders who train and employ GPOs.
Supervised upskilling placements
Rural Health West, WA ‘s rural workforce agency, co-ordinates an extensive GPO upskilling placement program in high volume obstetric units. This program supports GPOs to attend tertiary and secondary maternity hospitals for one to two weeks of intensive upskilling to maintain GPO skills.
Rural GP Obstetric & Gynaecology forum
This new professional development program, run annually over a weekend, is designed to provide GPOs with the opportunity to fulfil their CPD requirements and maintain credentialing with WA Country Health Services.
GP Obstetrics Think Tank
An annual evening event held in Perth that brings together a range of stakeholders invested in supporting GPOs. This allows networking, presentation of relevant information to GPOs and discussion about potential solutions to issues.
WA GP Obstetric Network
WAGPON was established in 2011 to provide a safe and nurturing space for GPOs to support one another and maintain strong morale amongst the GPO workforce. WAGPON has a website (www.wagpon.com.au) and sends a monthly email newsletter with relevant educational events, upskilling opportunities, job opportunities and locum work. WAGPON also aims to inform medical students and junior doctors about training and career opportunities.
In summary, GPOs are an essential part of Australian maternity services, providing integrated, continuity of care to women and their families in both country and city settings. GP obstetrics must continue and it is incumbent upon us all to find and implement solutions to the issues that confront it.
References
- Donnolley N, Butler-Henderson K, Chapman M, Sullivan E. The development of a classification system for maternity models of care. Health Inf Manag. 2016;45(2): 64-70.
- RANZCOG. Certificate in Women’s Health & DRANZCOG Melbourne: College House; 2019. Available from www.ranzcog.edu.au/training/certificate-diploma
- Sandall J, Soltani H, Gates S, et al. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev 2016;28(4):CD004667.
- Sandall J, Soltani H, Gates S, et al. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev 2016; (4): CD004667.
- COAG Health Council. Woman-centred care Strategic directions for Australian maternity services [Internet]. Canberra: Australian Department of Health; August 2019 [cited 29/3/21] Available from https://www.health.gov.au/sites/default/files/documents/2019/11/woman-centred-care-strategic-directions-for-australian-maternity-services.pdf







Leave a Reply