After years of controversy, countless studies and statements from specialist societies, where are we now with mid-urethral slings?
Incontinence of urine affects one in three 1 Australians. The economic impact of incontinence in Australia in 12 months is $42.9bn2 (2010, adults over 15 years of age). Approximately 65 per cent of women with incontinence will have stress urinary incontinence (SUI). SUI is a highly prevalent condition of involuntary urine leakage when the intra-abdominal pressure exceeds the urethral pressure typically associated with coughing, sneezing or exertion. SUI may impact significantly on quality of life, preventing many daily activities and limiting involvement in exercise and sport.
While SUI may occur in nulliparous women, it is more commonly associated with childbirth. The cause is presumed to be weakness in the pelvic floor structures, including disruption of the pubourethral ligaments and damage to connective tissue and muscles of the pelvic floor. The symptoms of SUI may, however, be caused by detrusor overactivity and intrinsic sphincter deficiency. This must be considered when planning treatment strategies as treatment needs to be based on correct diagnosis. It is not unusual to have a combination of problems leading to incontinence.
Commonly, intrinsic urethral sphincter deficiency (ISD) is included as SUI. ISD is defined urodynamically as a valsalva leak point pressure (VLPP) <60cm H2O or a maximum urethral closure pressure (MUCP) <20cm H2O.3 One may argue there is a significant difference between SUI owing to rotational descent of the urethra and/or pelvic floor dysfunction and symptoms of SUI owing to weakness of the urethral sphincter. ISD presents a particularly difficult group of patients who are at high risk of failure of current surgical techniques for SUI.
Diagnosis of SUI is by detailed history, examination, confirmation of complete bladder emptying and by exclusion of urinary tract infection and other lower urogenital tract pathology – commonly atrophic changes and coexistent prolapse. A urinary output chart is mandatory and provides much information. The recording of small frequent voids may indicate detrusor overactivity rather than uncomplicated SUI. Polyuria may indicate previously undiagnosed diabetes and this obviously needs exclusion. More commonly, bad habit with excessive fluid intake is the reason for the polyuria and before any decision on surgical management the urine output must be restored to normal (1.5L/24hrs).
Further investigation with urodynamic studies may be considered if there is any question about the diagnosis of uncomplicated SUI. It is interesting that there are very few situations where it is permissible to perform elective surgery without full and appropriate investigation.
Conservative management strategies should generally be considered before surgical intervention and may be instituted before urodynamic evaluation. These include: lifestyle changes; pelvic floor re-education; use of local oestrogens where appropriate; and weight loss in patients with a high BMI.
In spite of conservative management strategies, many women will require surgical intervention for more definitive control of the SUI. Since the mid-1990s, there have been significant changes in the surgical management of stress incontinence. The ‘gold standard’ colposuspension procedure, which had served well as a very successful operation for SUI, was challenged by the development of mid-urethral slings (MUS). These slings were readily adopted– being less invasive and associated with much faster recovery.
Fortunately, they have proven to have very satisfactory success rates both in the short and long term with minimal complications – fortunate because the rapid uptake of the use of MUS in general preceded adequate data and understanding of the ideal structure and weave of the tension-free vaginal tapes (TVTs).
The answer to the question of how the mid-urethral sling procedure works is not clear, but the presumption is that the sling corrects anatomic support of the urethra and may additionally provide a degree of compression to the urethra.
Recent controversies
Although the treatment of SUI with mid-urethral slings has been universally adopted throughout the world, there have been attempts by certain legal firms to associate the use of MUS to the controversies related to the US FDA release in 2011 of a white paper44 expressing concern regarding the transvaginal placement of mesh for prolapse.
Various influential organisations, including RANZCOG and the Urogynaecological Society of Australasia (UGSA), the International Urogynecological Association (IUGA), the American Urogynecologic Society (AUGS) and the Society of Urodynamics, and the Society of Urodynamics Female Pelvic Medicine and Urogenital Reconstruction (SUFU), have released statements strongly supporting the current widespread use of mid-urethral slings for stress incontinence.5 6
There has been considerable evolution with mid-urethral slings procedures during the last 15 years. Early multi-filament tapes were found to be associated with higher complication rates and discontinued in favour of uncoated, monofilament lightweight macroporous tapes.7 8 Initial MUS procedures involved a retropubic (RP) approach to sling placement. Subsequent development included transobturator (TO) placement of the tape and, more recently, the single-incision ‘mini slings’.
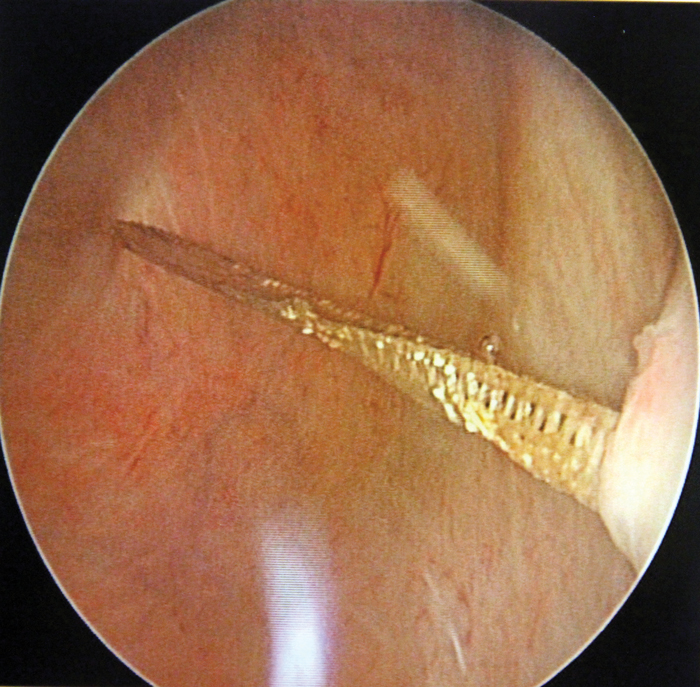
Figure 1. Failure to recognise RP tape traversing the bladder on the left side after perforated tape removed on the right (photo by Dr I Tucker)
Retropubic MUS
For many clinicians, RP mid-urethral slings remains their preferred option. Credit for the introduction of mid-urethral slings procedures is often given to Ulmsten and Petros. It may be argued that the original innovators were Raz and Stamey as it was their procedures that introduced the concept of mid-urethral surgical approach.
From the original ‘bottom to top’ approach of the TVT procedure developed the ‘top down’ Sparc procedure and there have been several ‘clones’ developed subsequently. The TVT and Sparc procedures, however, have the most data and are, arguably, the most studied of all gynaecological procedures. There have been some studies suggesting the TVT approach is superior to the Sparc, but the differences are less obvious in other studies, suggesting both procedures are successful and safe. 9 10 11
There is evidence that the RP approach may be indicated if the patient has coexistent ISD 12, but these data were obtained from earlier studies that also suggested more minimally invasive slings were less effective. More recent data dispute this and more studies are required.
RP mid-urethral slings procedures have been extensively studied and long-term effectiveness of up to 80 per cent has been demonstrated in studies following the patients for up to 17 years.13 14
RP slings are not without risk and entering the retropubic space can be hazardous. There is a significant risk of bladder perforation, a risk of bowel and intestinal perforation and a risk of haemorrhage and post-operative voiding difficulties. Owing to the risk of perforation of bladder and bowel, RP procedures should not be carried out is there has been a previous colposuspension or extensive retro-pubic surgery. Figure 1 shows a left sided bladder perforation present even though the surgeon had discovered and removed a right sided bladder perforation from the retropubic tape insertion. As always, correct surgical technique is essential. The incidence of postoperative voiding dysfunction seems to be greater with RP mid-urethral slings procedures, but it must be remembered that not all postoperative voiding difficulties are related to obstruction from the sling. Nevertheless, RP MUS remains popular and successful. As a result of the above possible complications, the TO approach to sling placement was developed.
TO MUS procedures
Insertion of the mid-urethral sling via the obturator foramen was introduced by Delorme in 2001.15 This ‘inside-out’ trans-obturator approach avoids the retro-pubic space thus reducing the incidence of bladder, bowel and intestinal perforation. Studies also suggest a reduced risk of postoperative voiding difficulties. There have been some criticisms regarding the lateral extent of placement of the tape and associated groin pain. de Leval et al 16 introduced a more medial ‘outside-in’ approach. Both approaches are associated with very acceptable success rates between 77–91 per cent. There have been several ‘clones’ of the ‘outside-in’ approach.
Recent studies also suggest similar success rates for the TO MUS as for RP MUS 17 and even question the previous suggestion that RP MUS procedures are the procedures of choice when there is coexistent ISD. There seems similar efficacy between the two well-studied procedures – Monarc and TVT-O.18 These TO MUS procedures, however, still require both vaginal and skin incisions.
Single-incision mini slings
In an attempt to further minimise the surgical approach to the treatment of SUI, The single-incision technique was developed. This technique avoids any external skin incision and utilises a shorter length of tape.
Two approaches were initially developed: the TVT Secur and the MiniArc. The TVT Secur was abandoned owing to reported higher incidence of failure but the MiniArc/MiniArc Precise/MiniArc Pro MUS procedures remain in current use. These procedures are associated with less pain and haemorrhage.
Initial studies suggested success rates below that of other MUS procedures, but more recent studies following a slight modification of the technique have shown very acceptable success rates.19 20 21 Essentially, the tape is left a little more ‘snug’ around the urethra rather than in the ‘tension free’ RP MUS procedure.
With this procedure, there is very little chance of bladder perforation, minimal risk of haemorrhage and postoperative pain is minimal. It appears that the original criticism of the single-incision mini-slings is likely to have been premature and unjustified.
Treatment of ISD
Traditionally, peri-urethral bulking agents have been offered to patients with this very difficult problem. While failure rates remain significant, there is evidence that RP MUS procedures may be effective for ISD. This is confirmed with several studies including those by Schierlitz et al12, Jeon et al22 and Araco et al23 all showed significant success rates in this cohort. These studies also suggested that RP mid-urethral slings were more successful than TO procedures when ISD was present. Other studies have produced contradictory results. Studies by Costantini E et al2424 failed to show any significant difference in outcome for ISD between RP MUS and TO procedures.
Treatment failures and complications
Current data suggest the failure rate for all MUS procedures is comparable. Failures are likely to occur because of:
- inadequate surgical technique;
- coexistent ISD;
- coexistent detrusor overactivity;
- occurrence of excessive exertion postoperatively and beforeadequate tissue ingrowth;
- high BMI; and
- other co-morbidities, such as excessive coughing, trauma and so forth.
Bladder perforation is largely a feature of RP MUS while groin pain is more commonly associated with TVT-O. Vaginal tape exposure is associated with all the procedures as is ‘button-holing’ of either anterior vaginal sulcus. Haemorrhage associated more with the RP MUS and occasional groin haemorrhage with TO MUS procedures.
Management of treatment failures
All patients with treatment failure require full assessment, including urodynamic evaluation and urethral pressure profilometry. The subsequent management will clearly depend on the results of the overall assessment.
Repeat surgery may confidently be offered to those patients with persistent SUI and this surgery may be a repeat of the previous operation or an alternative. A RP MUS procedure in the presence of sphincter deficiency may be a preferred option, although in those patients consideration may also be given to the injection of a peri/trans urethral bulking agent.
Tape exposures are usually relatively easily excised. Postoperative voiding dysfunction is more problematic as the question of loosening or cutting the tape needs consideration if it is certain that the voiding difficulty is related to obstruction from the tape.
Discussion
The procedures that have been most studied include the RP TVT and Sparc MUS procedures, and more recent with less longterm data are the TVT-O and Monarc MUS procedures and the MiniArc Precise procedure. With the most recent data, all have very acceptable success rates. It may not be appropriate to apply these success rates to the ‘clones’. The risk of tape exposure is present with all techniques but the incidence is low and acceptable. Pain is less with the more minimally invasive procedures as is postoperative voiding difficulty. Bladder/bowel perforation and significant haemorrhage are most likely to occur in the RP MUS procedures. All may be repeated should a failure occur.
Present data suggest that the three approaches are all satisfactory and may be considered as surgical options. The position statements by the various organisations representing urologists, urogynaecologists and gynaecologists have been authoritative, factual and totally supportive of the use of mid-urethral slings for the surgical management of stress urinary incontinence. These statements have emphasised that MUS procedures have been objectively studied more than any other gynaecological procedure and have undeniable success rates, very low complication rates and exceptional patient acceptance.
Conclusion
When the surgical option for stress incontinence is entertained, the choice of procedure will be up to the patient and the surgeon following full and complete explanation and confirmation that the condition of stress urinary incontinence exists. The surgeon may choose the procedure he/she is most experienced with and deems the most appropriate for the situation.
The importance of adequate training/mentoring/proctoring and credentialing is paramount to ensure that all surgeons are not only performing these surgeries at the highest standards, but are also performing surgery as the correct option for the correct reason. There is far more to operating than just the practical aspect. We are fortunate to have these very safe and successful MUS procedures allowing a well-tolerated and accepted, minimally invasive approach to the surgical management of stress urinary incontinence.
Conflict of interest statement
Dr Tucker has no conflicts of interest to declare. Current appointments include the following: Urogenital Prosthesis Clinical Advisory Group (UPCAG) of the Australian Federal Government Department of Health; National Vice President and Member of the Board of Directors of the Continence Foundation of Australia; Member of the Advisory Board of UGSA (Urogynaecological Society of Australasia); Member of the International Advisory Board of Acta Obstetricia et Gynecologica Scandinavica; Member International Advisory Board for Boston Scientific with Dr Peter Rosenblatt, Dr Karen Noblett and Dr Sandip Vasavada; Member of IUGA; Member of ICS; Member of the International Neuromodulation Society; and Secretary of the Audio-Engineering Society (Adelaide Section).
References
- www.continence.org.au/pages/key statistics.html
- www.continence.org.au/data/files/Access_economics_report/dae
- Sand PK, Bowen LW, Panganiban R, Ostergard DR. The low pressureurethra as a factor in failed retropubic urethropexy. Obstet Gynecol.1987 Mar;69(3 Pt 1):399-402
- Urogynecologic Surgical Mesh: Update on the Safety and Effectivenessof Transvaginal Placement for Pelvic Organ Prolapse. [FDA].
- http://www.sufuorg.com/News/Announcements/SUFU-and-AUGSRelease-Position-Statement-on-Mesh-M.aspx
- Position statement on midurethral slings UGSA, RANZCOG www.ranzcog.edu.au/doc/position-statement-on-midurethral-slings-c-gyn-32.html .
- Rapp DE, Kobashi KC. The evolution of midurethral slings. Nat Clin Pract Urol. 2008;5:194–201. [PubMed: 18317496].
- Kaven Baessler Royal Women’s, Mater and Wesley Hospitals Brisbane, QLD, Australia. Obstetrics and Gynecology 11/2005; 106(4):713-6. DOI: 10.1097/01. AOG.0000177970.52037.
- Andonian S, Chen T, St-Denis B, Corcos J. Randomized clinical trial comparing suprapubic arch sling (SPARC) and tension-free vaginal tape (TVT): One-year results. Eur Urol. 2005;47:537-41. [PubMed: 15774255
- Nazemi TM, Yamada B, Govier FE. Minimum 24-month follow-up of the sling for the treatment of stress urinary incontinence. J Urol. 2008;179:596-9.
- Primus G. One year follow-up on the SPARC sling system for the treatment of female urodynamic stress incontinence. Int J Urol. 2006;13:1410-4.
- Schierlitz L, Dwyer PL, Rosamilia A, Murray C, Thomas E, De Souza A, et al. Effectiveness of tension-free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency. Obstet Gynecol. 2008;112:1253-61.
- Nilsson CG, et al., Seventeen years’ follow-up of the tension-free vaginal tape procedure for female stress urinary incontinence. Int Urogynecol J, 2013. 24(8): p.1265-9ISRN Urology
- Svenningsen R, Staff AC, Schiøtz HA, Western K, Kulseng-Hanssen S. Long-term follow-up of the retropubic tension-free vaginal tape procedure. Int Urogynecol J. 2013 Aug;24(8):1271-8
- Delorme E, Droupy S, de Tayrac R, Delmas V. Transobturator tape (Uratape): A new minimally-invasive method in the treatment of urinary incontinence in women. Prog Urol. 2003;13:656-9.
- de Leval J et al. Novel surgical technique for the treatment of female stress urinary incontinence: Transobturator vaginal tape inside-out. Eur Urol. 2003;44:742–30
- Costantini E, Albo ME, Zyczynski HM, Kenton K, Norton PA, Sirls LT, et al. Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med. 2010;362:2066-76.
- Liapis A, Bakas P, Creatsas G. Monarc vs TVT-O for the treatment of primary stress incontinence: a randomized study. Int Urogynecol J Pelvic Floor Dysfunct. 2008 Feb;19(2):185-90.
- Lee J, Rosamilia A, Dwyer P, Lim Y, D Ulrich,MiniArc, Monarc suburethral sling in women with SUI an RCT – 24m results IUGA 2014.
- Schellart RP, Oude Rengerink K, Van der Aa F, Lucot JP, Kimpe B, de Ridder DJ, Dijkgraaf MG, Roovers JP. A Randomized Comparison of a Single-incision Midurethral Sling and a Transobturator Midurethral Sling in Women with Stress Urinary Incontinence: Results of 12-mo Follow-up. Eur Urol. 2014 Aug 25. pii: S0302-2838(14)00679-4. doi: 10.1016/j. eururo.2014.07.027. [Epub ahead of print].
- Rui Oliveira, Alexandre Resende, Carlos Silva, Paulo Dinis, and Francisco Cruz, Mini-Arc for the Treatment of Female Stress Urinary Incontinence: Long-Term Prospective Evaluation by Patient Reported Outcomes, ISRN Urology Vol 2014 (2014), Article ID 659383.
- Araco F, Gravante G, Sorge R, Overton J, De Vita D, Sesti F, et al. TVT-O vs TVT: A randomized trial in patients with different degrees of urinary stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:917-26
- Jeon MJ, Jung HJ, Chung SM, Kim SK, Bai SW. Comparison of the treatment outcome of pubovaginal sling, tension-free vaginal tape, and transobturator tape for stress urinary incontinence with intrinsic sphincter deficiency. Am J Obstet Gynecol. 2008;199(76):e1-4.
- Costantini E, Lazzeri M, Giannantoni A, Bini V, Vianello A, Kocjancic E, et al. Preoperative valsalva leak point pressure may not predict outcome of mid-urethral slings. Analysis from a randomized controlled trial of retropubic versus transobturator mid-urethral slings. Int Braz J Urol. 2008;34:73-83.




Leave a Reply