Women’s Health Circle acknowledges the traditional custodians past and present on whose land we walk, work and we live including the Bindal and Wulgurukaba People of Townsville, Bwgcolman people of Palm Island and the Lardil, Gangalidda, Waanyi, Garrawa and Yunjulla peoples of the Southern Gulf of Carpenteria.
If you were to draw a hypothetical line from the Tropic of Capricorn across Australia, you would see a significant disparity in maternal, fetal, and neonatal outcomes in Northern Australia with fewer resources, personnel, and perinatal specialists to manage the increased morbidity and mortality as shown in Figure 1.
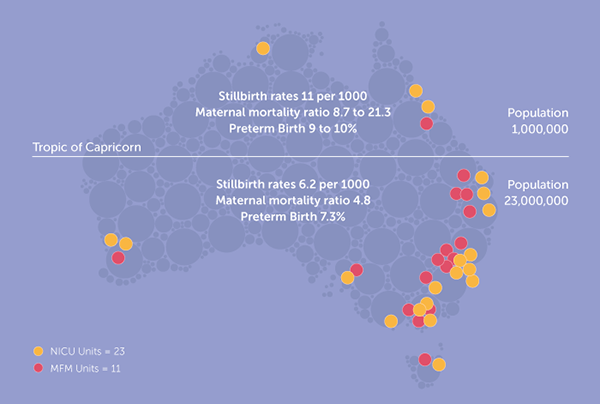
Figure 1. Number of NICU and MFM Units across Australia
There are many contributing factors, including the environmental diversity, wet seasons, restricting travel and access, low population numbers and density, a higher proportion of First Nation peoples living remotely, food insecurity, along with the significant distances to access health care.
The vast distances that women living in remote Australia have to travel for routine pregnancy care and ultrasound is unfathomable. It can be a minimum of one or two flights on commercial aeroplanes (which often have significant delays), or 5 to 8 hours by car with limited options for accommodation en route – notwithstanding the financial burdens and transportation challenges faced once women and their families arrive in town.
Things that we take for granted include the need to get transport out of hours, to and from the airport and their accommodation and then travelling to the health services in time for appointments, the cost of food while women are away, not to mention the fact that many women do not get to bring an escort or have a family member with them during their travel times for routine ultrasound and pregnancy care. For a young 16-year-old woman living on Mornington Island in the Gulf of Carpentaria, in her first pregnancy, these barriers are prohibitive to accessing routine ultrasounds at the correct gestation.
Our story began on Palm Island over 20 years ago, when a sonographer and midwife team, Sue Bloomfield, and Alexandra Gosden, established a monthly visiting sonography service via Queensland Health to compliment the visiting midwifery services.

In the last 4 years, I became involved as a visiting obstetrician/sonologist to Palm Island to facilitate the timely reporting of ultrasound scans, appropriate management of abnormal ultrasound findings, and to provide higher risk models of care to prevent women from travelling back and forth. This evolved into the development of pregnancy screening to prevent obstetric complications, working collaboratively with the local medical service through the Palm Island Community Council. Check Up Australia funded additional visits for both obstetric care, sonography, and gynaecology visits.
Other remote communities in the Gulf of Carpentaria approached Check Up Australia with a request for a similar service, and we were engaged to formally establish the Care on Country Program The communities included Mornington Island, Normanton, Karumba, Doomadgee and Burketown, from which 96% of women usually deliver at Mount Isa Hospital in Mornington.
The aim of the Care on Country program is to:
- Connect women and their families to their pregnancies through the use of ultrasound.
- Reduce the need to travel for routine pregnancy ultrasounds.
- Train local staff in how to use the ultrasound machine for point of care and to perform a basic dating scan in order to facilitate an estimated gestation and due date.
- Primary and secondary prevention of obstetric complications such as pre-eclampsia and preterm birth.
We are now 18 months into the program, which has evolved to embrace state-of-the-art digital technology. We use a combination of satellite internet (Starlink), web-based practice management software that can be accessed anywhere and the use of cloud-based picture archiving and communication systems (Cloud-based PACS). The ultrasound images are performed on a portable ultrasound made by General Electrics (GE). We have also integrated artificial intelligence (AI) to improve the efficiency of documentation and reporting. Women can either get their photos printed out or receive them directly on their smart phones.
In the first 12 months, from July 2023 until the end of June 2024, we have seen over 308 women in the Gulf of Carpentaria, with 250 obstetric related visits and 59 women were seen for gynaecology. The majority of ultrasounds performed in the communities were second and third trimester ultrasounds. We were able to perform 28 combined first trimester screenings using the Fetal Medicine Foundation algorithm for both aneuploidy and placental dysfunction, early onset pre-eclampsia. We also perform routine cervical screening at the time of morphology in line with the Preterm Birth Alliance’s recommendations. We work collaboratively with the outreach midwifery group practice service, the O&G teams at the base hospital, the local Aboriginal medical services, and the local hospitals.
At least one third of women seen in the Gulf communities in this period, were classified as high risk based on a maternal, fetal, uterine, cervical or a placental issue. Overall:
- 59% of ultrasounds were classified as normal.
- 5% of reviews were related to miscarriage and termination of pregnancy requests.
- 3% of fetuses had a structural abnormality found.
- 7% showed placental dysfunction including late onset placental insufficiency, fetal growth restriction, oligohydramnios, or pre-eclampsia.
- 4% of women were found to have an asymptomatic short cervix. At diagnosis, these women were commenced on progesterone at the time of the ultrasound and were followed up for cervical surveillance at the maternity hospital.
- 8% of women had pre-existing medical conditions, such as rheumatic heart disease, ischaemic heart disease, goitre, and other health issues present at the start of pregnancy.
- 3% of pregnancies were complicated by pre-existing or gestational diabetes, large for gestational age, and/or polyhydramnios.
There are always challenges to overcome with any new program. The unpredictable wet season and multiple cyclones last summer in the north of Australia, resulted in the last-minute postponement of our trips. Despite this, we were able to do catch-up visits and community engagement remained high, as shown in Figure 2.
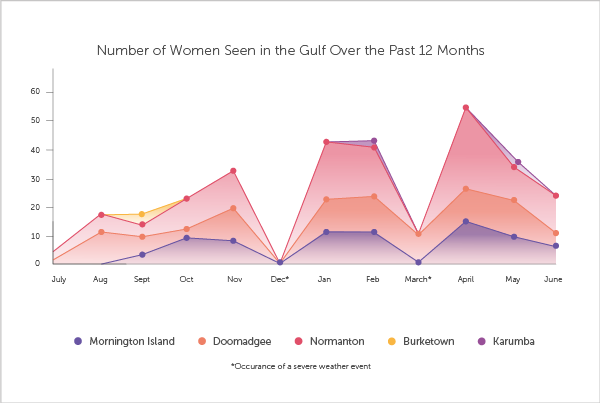
Figure 2. Impact of weather events on patient visits
One of our biggest challenges was poor mobile reception which led to unreliable connectivity to the internet, impacting our ability to upload images to our cloud-based server and perform timely reporting. This has been partially resolved by using satellite technology which provides high speed internet anywhere. Our reporting efficiency will be aided by the advent of a web-based viewpoint in the near future.
In its first 12 months, our program has been estimated to save the healthcare system over $2 million in the transportation of women for routine antenatal care and ultrasound. The cost benefit ratio calculated using the Australian Social Bank Value based on the reduction in parental stress through the Care on Country program is 8.7. This means for every $1 spent on this program, there is a cost savings of $8. Not to mention the benefits of improved outcomes from pregnancy screening and treatment to prevent early onset pre-eclampsia and preterm delivery.
There is no doubt the greatest part of the program is experiencing the delight and excitement generated when a woman sees her baby on ultrasound in their home community for the first time. To be able to share this moment with their children and families has been the highlight for us.
It is such a privilege and honour to meet these amazing families, local staff, the wonderful midwifes and provide access to services such as routine obstetric and gynaecology ultrasound and pregnancy care on Country.
To conclude, the statement from the International Society of Ultrasound in Obstetrics and Gynaecology (ISUOG) summarises our mission to achieve equity in women’s imaging. ‘All women should have access to ultrasound, that all scan providers are competent and that all O&G conditions are effectively diagnosed’.
Connecting women and their families who live remotely to their unborn baby using the portable ultrasound technology is truly special. We are one step closer to achieving equity and the future of outreach women’s imaging is so exciting.
If anyone is interested in the program, we would love to hear from you. Please email me at [email protected]
References
ITN Online. (2023). The emergence of cloud-based PACS and other trends. Imaging Technology News. https://www.itnonline.com/article/emergence-cloud-based-pacs-and-other-trends




Leave a Reply