RANZCOG’s Obstetrics and Gynaecology Education and Training Program, better known as OGET, has reached a significant milestone, welcoming its 1,000th participant in December 2023. The program, funded by the Federal Government and led by RANZCOG, delivers upskilling and education to a range of health professionals involved in providing maternity and gynaecology services. Primarily focusing on Monash Modified Model (MMM) areas 2 to 7, OGET is a multi-disciplinary program that takes a collaborative learning approach, helping to facilitate the safe and equitable provision of maternity and gynaecology services in rural, regional, and remote areas.
The OGET journey
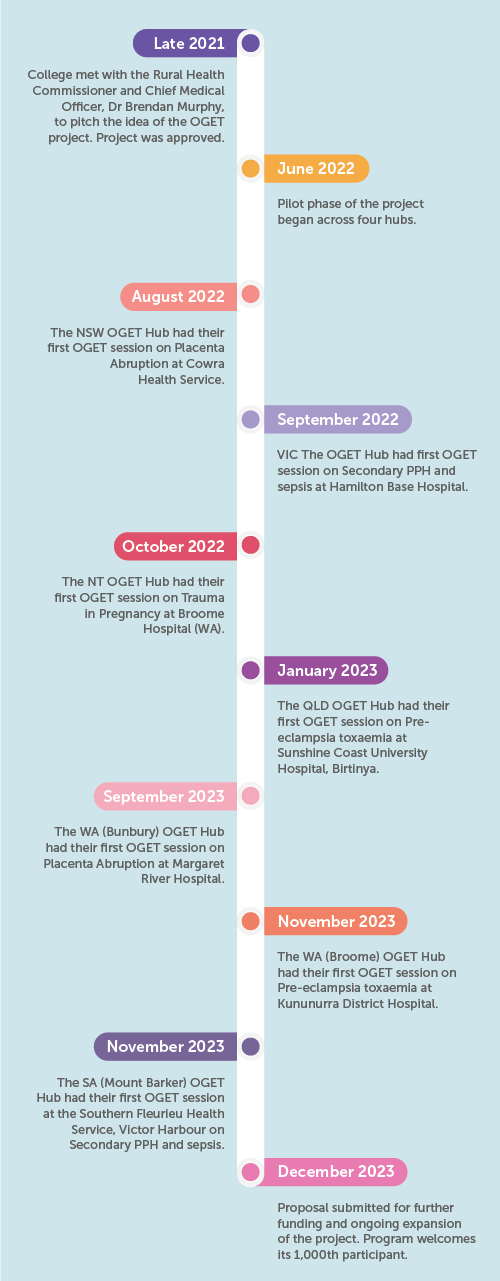
OGET began its journey in 2022 with a pilot program and the establishment of four regional hospital hubs in Warrnambool (VIC), Sunshine Coast, (QLD), Darwin (NT), and Orange (NSW). These hubs offered onsite and outreach training to nearly 20 peripheral rural and remote health services through case-based learning and interactive forums. In addition to clinical skills, the training also addressed other critical skills such as cultural competence, leadership, communication and wellbeing, both from a practitioner and a patient perspective. During this pilot phase, the program helped train and upskill over 250 GPs, registrars, anaesthetists, midwives, nurses and other health professionals.
Recognising the success of the pilot phase, the Federal Government committed further funding in 2023 to expand the program until February 2025. This led to the development of four more hubs in Bunbury (WA), Broome (WA), Toowoomba (QLD), and Mt Baker (SA), increasing the number of rural and remote hospitals supported from 20 to 33. In addition to increasing the number of training health service sites, the funding also covers the purchase of simulation equipment, enabling health professionals to learn and practice in a safe and risk-free environment.
Today OGET is credited to have trained over 1,000 participants and counting, firmly earning its place as one of RANZCOG’s most successful rural workforce initiatives.
The people behind the program
RANZCOG is committed to ensuring that OGET is led strategically and operationally by a diverse group of health professionals with an understanding of rural and remote women’s health. The OGET governance structure includes:
- The OGET Steering Committee – The Committee reports to the RANZCOG Board and is chaired by Associate Professor Jared Watts, a rural O&G from Broome (WA). The Committee has Fellow and GPO representation and oversees the strategic delivery of OGET, ensuring that the program meets its set objectives.
- The Resource Development Working Group – The Working Group reports to the OGET Steering Committee and is chaired by Dr Elisha Broom, a Fellow from QLD (a position previously held by Associate Professor Ted Weaver who led the OGET Sunshine Coast, QLD Hub). The Group has Fellow, GPO and midwifery representation and develops educational resources used by the OGET Hubs, with a focus on creating scalable resources that can be customised and replicated across a diverse range of health care settings. This includes case studies, videos, workshop content and e-learning modules.
To help keep the OGET wheels turning, the program relies on dedicated Fellows, GP Obstetricians, and College and hospital administration staff to ensure that the College delivers high quality education to its participants. Each hub also has a dedicated OGET FRANZCOG Lead who leads on the delivery of the program locally.
Improving the workforce
The impact OGET has had on the rural maternity and gynaecology workforce is clear, with participants often expressing how valuable the OGET sessions are for their clinical practice. Participants have reported an increase in confidence levels at the end of each session based on their knowledge of the case topic, scope of practice in managing similar types of cases, and their ability to contribute meaningfully as a member of a team managing the case. OGET case topics include Trauma in pregnancy, Difficult birth, Missed antenatal result, Mental health, Renal issues, and Threatened preterm labour in a rural location.
Dr Jake Parker, a GP Obstetrician based on Thursday Island, and a member of the OGET Resource Development Working Group, describes how the program was developed specifically for the rural workforce:
“The OGET program has been designed with the education needs of Australian rural and remote maternity units in mind. With input from both specialist FRANZCOGs and General Practitioner Obstetricians, the OGET program aims to deliver high-quality maternity education sessions that are both contextualised to the rural hospital setting and can be delivered close-to-home. It delivers case studies which explore issues specific to managing obstetric and gynaecological cases in rural and remote Australia, including retrieval medicine.”
RANZCOG has also taken into consideration the importance of multi-disciplinary learning as a form of integrating the knowledge, skills, and perspectives of the diverse range of health professionals that play a key role in the delivery of maternity and gynaecology care. This is crucial for rural and remote areas, as the successful delivery of maternity and gynaecology care relies not only on O&G specialists, but also GP obstetricians, anaesthetists, midwives, and other health professionals.
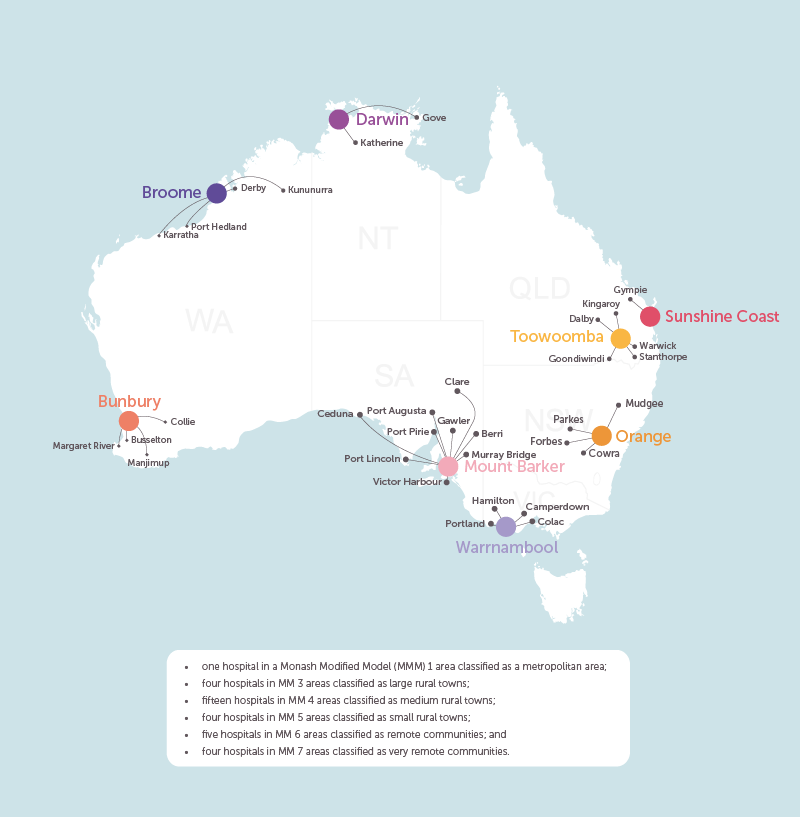
Regional hub map of OGET sites. Remoteness and population size measured on a scale of Modified Monash (MM) categories.
OGET reflections
“The OGET project has enhanced my relationship with the other hospitals in my area in so many ways and allowed me to get to know many clinicians I would not otherwise have met, from Obstetricians, GP Obstetricians and midwives to theatre and ward staff and anaesthetists. This has a massive advantage when we are discussing difficult clinical situations as we often already know each other’s thoughts and capacities. I think the learning around the cases is a two-way street, and I have learnt a lot teaching them. We have had some fantastic group discussions over the course of the OGET project.”
Dr Rosy Buchanan, OGET Warrnambool (VIC) Hub Lead
“OGET has really helped develop the relationships between larger regional hospitals and the smaller units they support. It has allowed consultants and GPs who for years have discussed patients over the phone to actually meet in person for the first time. The consultants have then been able to see the local services and resources available in peripheral units who they are giving advice to.”
Associate Professor Jared Watts, OGET Steering Committee Chair
“As a clinical midwife it’s helped me understand what A/N screening should be ordered by GPO in obstetric clients at risk of PE and allows me to understand what markers are crucial to observe and be more vigilant with.”
Program participant
“Appreciate how interactive (the session) was & that the presenter was open to education from the audience.”
Program participant
“I just wanted to say what a fabulous study day it was today! So informative!”
Program participant
OGET in numbers
- OGET supports 33 rural and remote Australian health services from eight (8) regional hospitals
- 28 of the 33 OGET peripheral OGET health services are in medium and small rural towns (MM4 and 5), remote communities (MM6) and very remote communities (MM7)
- The largest self-reported OGET cohort is midwives at 44%
- The second largest self-reported OGET cohort is nurses at 15%
- The third largest self-reported OGET cohort is General Practitioners at 11%
What’s next?
Despite the overall success of OGET, there is still much work to be done to improve access to maternity and gynaecology services in areas of need. The growth and evolution of OGET relies on participant feedback, and despite an overwhelming number of positive responses received, there is always room for improvement.
A proposal to the Federal Government was submitted by the College in December 2023 for further funding. This proposal looks to expand the program at the end of the project funding period in February 2025. The expansion of OGET to establish more hubs will help ensure the equitable provision of similar training opportunities for more rural and remote health services.
Further changes are happening from an education and learning perspective. ‘The program is expanding its resources to include obstetric skills sessions and will be further tailored using direct feedback from participants,’ says Dr Parker.
RANZCOG has also identified the need to provide more sessions, and to continually review their distribution, so that geographically isolated rural and remote health services receive more dedicated training and upskilling opportunities. Ongoing funding and support will help to ensure more health services in medium and small rural towns, remote communities, and very remote communities are part of the proposed OGET expansion.
With continued support from its participants and enthusiasm of its team members, the future of the program looks bright. Provided the recent Federal Government proposal is successful, the program will continue to evolve and better align with the needs of its participants and the communities they serve.
To find out more about OGET, please email the OGET team at [email protected].





Leave a Reply