Close your eyes and give me a definition of pain. That’s something we should be able to call to mind, right?1 Did you get sensory? Emotional? Actual or potential? I wonder about our ability to prevent and treat pain if we often struggle to define it. In this article, I’ll attempt to discuss the treatment of persistent pain before surgery in less than 1,500 words – no mean feat! Let’s start with:
- The more pain you have now, the more pain you are at risk of having in the future
- The better your pain is before an operation, the better it will be after
- Pain is made in the brain and felt in the body
- A bio psychosocial (spiritual) approach has a better chance of treating pain than an exclusively biomedical approach (social – health literacy, work, relationships, racism, loneliness, etc)
- There is a public health emergency of chronic pain in Australia and Aotearoa New Zealand: 1/5 adults
- 2017 was the International Association for the Study of Pain’s year of Pain After Surgery2 to educate clinicians and patients. Surgeons are well placed to reduce pain pre-op, so patients do better post-op
- National guidelines caution against using opiates for non-cancer pain
- Use questionnaires (American surgeon, writer, and public health researcher Atul Gawende says embrace the checklist!) to help you in your consult with knowledge and time, to teach the patient that you care about all their variables, and to help junior staff learn.
A bio psychosocial approach to pain
Ok, so you see a patient; you book them for a laparoscopy to investigate pain. Let’s use “the waiting list” as a “preparation list3” during this time and teach about a bio psychosocial approach to pain.
Less pain pre-operatively predicts less pain post-op – so will you try for amenorrhoea, anovulation? Down train painful pelvic floor muscles with stretches, breathwork and pain education with physio and other appropriately educated experts of the movement system? What about sleep? You need to consider quantity, quality and routine for a solid base of Maslow’s pyramid and for a quick screen for PTSD and yellow flags (i.e. nightmares).
Post-operative movement, once it’s safe to move the body, hastens recovery and opiates are good for pain at rest post-op but perhaps not to improve function. Exercise treats pain, encourage your patients to do more than before for the endocannabinoids. For many, exercising in the morning works better than later on in the day, as willpower can often decline as the day goes on. Exercising outside in nature is better for the immune system, and sunshine helps manufacture endorphins and endocannabinoids.
Think about nutrition as a powerful tool to help address the average person’s fibre deficiency, trial of low FODMAP for comorbid IBS, to limit constipation confusing the post-op picture4, and to treat depression5.
Is your patient trying to conceive? Zinc sulphate with periods6, tranexamic acid and non-steroidal anti-inflammatories could be suitable. Or a short course of amitriptyline pre-op to improve sleep and pain.
A psychological approach to pain
Mental illness is a common comorbidity in surgical patients and has a bidirectional association with pain. For non-life-threatening problems, we should tell our patients that we need to care for mind and body simultaneously, i.e. you cannot fix mental health first, then pain second, and vice versa.
Catastrophising is a popular area to study in medical literature as a predictor of pain, and I wonder to what degree doctors must take some responsibility for this characteristic. It describes someone who magnifies the threat value of their pain and feels helpless. Somehow this has never sat well with me. We have a role to play in acknowledging our patient’s suffering, being explicit about their pain being real, and moving away from an exclusive biomedical approach which can contribute to the sense of helplessness.
Check the patient’s beliefs, expectations and meaning of symptoms – have they got extra things going on? Neurodiversity? Gender diversity?
Additionally, plenty of psychological therapies are effective in treating pain, including pain where opiates are being prescribed7. These include Cognitive behaviour therapy (CBT), meditation and hypnosis. Eye movement desensitisation reprocessing (EMDR) also has increasing evidence for pain management, having originally been developed for treating PTSD. Just because we may not know where to access these treatments does not mean we shouldn’t tell our patients they exist. Then join forces with amazing patient advocates to fix our systems to provide access – they are a force to be reckoned with and can effect significant change in our society.

A social approach to pain
Loneliness is as bad for your health as 15 cigarettes a day says the US Surgeon General Dr Vivek Murthy. It’s a risk factor for pain. Options include social prescribing, participating in research8, joining moderated support groups, and getting your body moving in a group.
Pain neuroscience education treats pain9, and when we take a patient’s history, we should learn as we go. Yes, they might have endometriosis, yes that is a decent prolapse, but what happens if the endometriosis is only 5% of your suffering, and undertreated other things 50%? See pain curriculum below10.
Language can help treat pain – what you say in your consult has evidence for being therapeutic. Be a placebo, not a nocebo11.
But my patient has a 10cm cystadenoma on scan, you might say, and all she needs is a laparoscopic cystectomy, right? Or a really uncomfortable prolapse and a vaginal hysterectomy is what she needs, not meditation, right?
So, when the patient post-laparoscopic cystectomy has unexpected pain post-operatively and we discover she has had IBS for ten years, along with migraines, PTSD symptoms untreated after childhood trauma, and an awful work environment, we shouldn’t be surprised she ends up on ketamine for a week. Or the 55-year-old patient post vaginal hysterectomy and repair has no response to her operation for pain, despite an excellent anatomical result, and it turns out she has fibromyalgia, which predicts around 25% of people having a hysterectomy for pain will not respond to surgery12. Could a five second body map have helped? In short, yes. Let’s get the word out pre-op!
So, in summary, we can talk to the patient and use that Waiting List time as Preparation Time (taking a history, educating as we go – don’t forget that consult is a treatment; give them some notes to take with them as typically, only up to half of the discussion is remembered16), talk to the anaesthetist at time out about multimodal analgesia (more things IV), put on the music the patient
has chosen to go to sleep to reduce pain and opiate requests in recovery.
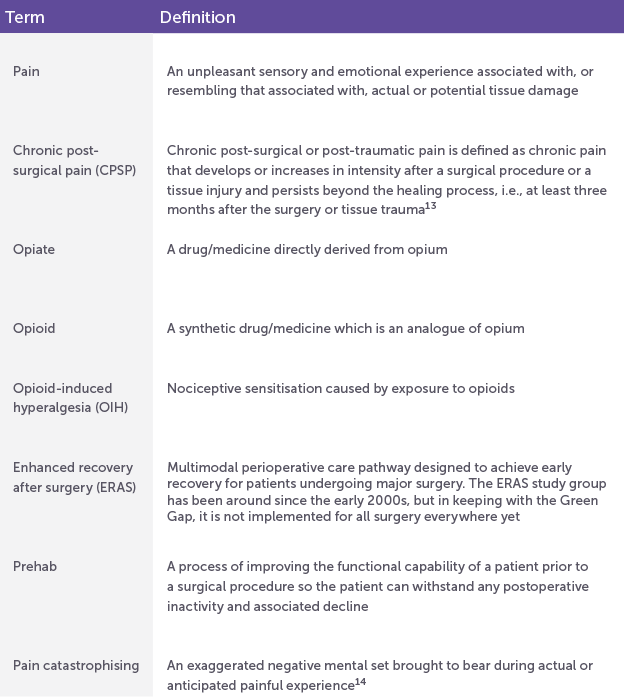
Helpful definitions
References
- Pain is “An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage” IASP 2020
- Pain After Surgery: What Health-Care Professionals Should Know
- With thanks to Dr Rachel Shanks, UHG
- E.g. CALHN PreHab – Getting Ready for Surgery
- The SMILES trial, Food & Mood Centre, Deakin University
- E.g. Obiagwu HI, et al. Efficacy of zinc supplementation for the treatment of dysmenorrhoea: a double-blind randomised controlled trial. J Int Med Res. 2023 May;51 (5)
- Garland EL, et al. Mind-Body Therapies for Opioid-Treated Pain: A Systematic Review and Meta-analysis. JAMA Intern Med. 2020 Jan 1;180(1):91-105.
- EndoZone
- Bless those Adelaidians, Dr David Butler and Prof Lorimer Moseley, who wrote Explain Pain.
- Meg Odgers’ Pelvic Pain and Sexual Pain Resources and Instagram: pelvicpain_researcher
- Thanks Dr Karin Jones, RWH
- As-Sanie S et al Incidence and predictors of persistent pelvic pain following hysterectomy in women with chronic pelvic pain. Am J Obstet Gynecol. 2021 Nov;225(5): 568.e1-568.e11
- Schug SA et al IASP Taskforce for the Classification of Chronic Pain. The IASP classification of chronic pain for ICD-11: chronic postsurgical or posttraumatic pain. 2019 Jan;160(1):45-52
- Sullivan 2001
- IASP – Terminology
- This can vary. Check the literature.




[…] Examples she shares include getting good sleep and regular exercise. […]