Long Acting Reversible Contraceptives (LARC’s) have significantly improved the range of contraceptive options. The Levonorgestrol IUS (Mirena) also has important uses for the management of menorrhagia and menopausal hormone therapy. I often think it is the best thing to come out of Finland after Nokia phones.
Unfortunately there are many negative comments in various media about Mirena and the insertion process, but the vast majority of recipients are very happy and return every five years for a change over.
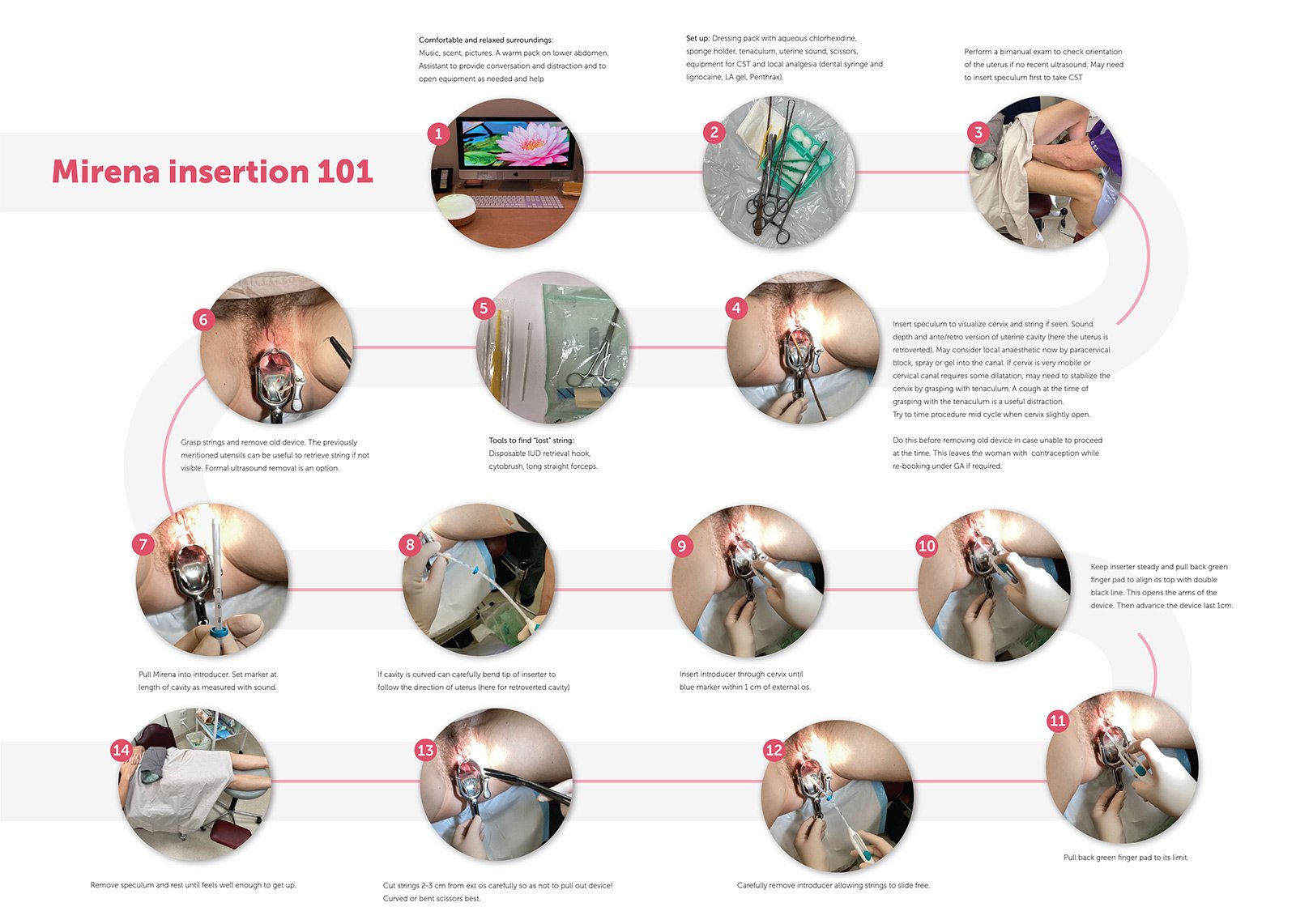
This step-by-step guide is intended as a description of one way to insert this device. After inserting hundreds (and having three myself), I have some practical tips to pass on, and have sought some useful ideas from other health practitioners. This paper shows how I replaced a Mirena in a patient who volunteered to be photographed as she is so satisfied with the device. Along the way I have mentioned things other doctors have suggested, and details of these can be explored further if interested.
For example not every clinic or consulting suite has access to ultrasound to check position or for difficult insertions. Various forms of pain relief or local anaesthesia can be used, from paracervical blocks, to intra cervical lignocaine, or topical spray. The “green whistle” of Penthrax is also useful if a degree of cervical canal dilatation is required, and perhaps a dose of non steroidal medication 30 minutes prior or some misoprostol if expecting a tight cervix can help.
Personally I find a well prepared patient in calming surrounds with a friendly assistant/nurse is all that’s usually required. This preparation includes a realistic explanation of the sensations during insertion, post insertion cramps that should be short lived, a description of the usual weeks of spotting and an appropriately timed pregnancy test before the procedure.
Some practitioners routinely use bedside ultrasound to check in cavity but this is not often available in many clinics. General post insertion advice is to get up slowly after resting for a few minutes and stay until comfortable to leave.
Simple analgesia may be required for a day but advised to contact inserter if worsening pain in next 24-48 hours that might suggest expulsion or translocation through the uterine wall if embedded during insertion.
Signs of infection such as pain, smelly discharge or fever over the next 2-3 weeks should be reported, or rarely pain noted by male sexual partner if strings have moved well up into the cervix leaving short sharp ends protruding.
I suggest a review visit for a string check after the next period or in 4-6 weeks to discuss bleeding pattern and look at length of string for future reference. Again some do a bedside ultrasound if available but if string not seen an ultrasound should be performed or arranged to check the device is in the cavity. If not seen in the uterus a plain x-ray should be done, and laparoscopic retrieval arranged with interval contraception. If the Mirena not found on x-ray the device may have been expelled during bleeding, especially if put in for menorrhagia and the first period full of clots.
If all well at this visit I don’t tell women to regularly feel for the string, but recommend not using a menstrual cup as this has been found to pull out a Mirena. Most women would not have enough bleeding to require a cup.
If the device is inserted in the first week of a regular cycle no other contraception is required but if later or uncertain, don’t rely on the Mirena for at least a week. The Federal TGA in Australia still has Mirena listed as working for five years, but in the US it is now used for five years for menorrhagia and eight years for contraception. Some sort of reminder of this time is worthwhile, such as an annual “Mirena birthday” on a phone, or if post partum remembering to replace when this child is approaching school age. For perimenopausal women who are not using it with oestrogen therapy I feel it could be safely left for at least six years, and by then regulators may have updated their advice.




Leave a Reply