Incivility carries many definitions across dictionaries; however, as demonstrated in Figure 1, negative connotations commonly associate themselves with this noun.

Figure 1. Definitions for Incivility.
It is hard to believe that a word like this can exist in our medical environment, especially when we consider where it derives from: the Latin world incivilis meaning ‘not of a citizen’.
Why is medicine vulnerable to incivility?
When we look at the environment in which we provide healthcare, it is no surprise that as medical professionals, incivility can encroach our everyday clinical shifts.
Those busy hours where everything is done at haste, where manners and simple courtesies are often neglected. The time demands and a pressurised healthcare system lead to long hours and fatigue. The next day brings endless referrals from another specialty, being paged in the early hours of the morning to chart simple analgesia, and frustrations of trying to start an operating list while the equipment ‘chooses’ to fail.
This list is not exhaustive, but the message is clear.
The environment in which we work can, by default, put us in situations where we are ‘uncivil’ to one another; abruptly snapping, passive aggressiveness, sniping comments or simply inappropriate workplace conduct and etiquette can occur easily and inadvertently or without deliberate malicious intent. The traditional hierarchical nature of our medical departments can also make us vulnerable to behaving in this manner, with teams being led by the more senior members of the consultant body followed by the tiered system of registrars and house officers.
Whether we like it or not, incivility occurs across medicine. For a multitude of reasons, it is hard to accurately quantify its prevalence and more significantly, its impact, on the medical workforce. However, we can assume it still exists when inferring other research findings.
The UK has been able to capture and provide evidence for incivility and its impact. In a survey conducted across 606 varied English medical doctors published in 2015, up to 40% of staff described rude, dismissive and aggressive communication had a ‘moderate-to-severe’ impact on their professional daily work, and 31% had been exposed to this behaviour multiple times a week.1 Only 7% reported they never experienced it.2
Whether as a country, a fraternity or a specialty, incivility is prevalent and has potentially significant repercussions on happiness at work, productivity and our capability to provide safe and high-quality healthcare.
What happens when one is uncivil?
Incivility has a profound impact on all those within the environment at the time the act occurred, as demonstrated in Figure 2.
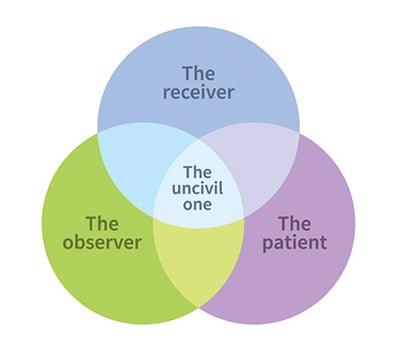
Figure 2. The relationship matrix of incivility.
1. The receiving individual
Rudeness (direct or passive) to one will cause stress to the receiving end, and subsequently result in diagnostic errors, technical performance, and delay in diagnosis and treatment.3 4 The mechanism is very simple; stress can inflict changes in one’s cognitive processing as well as provide distraction to the job at hand. In addition, one may engage in avoidant behaviours, lose focus and never complete the task.
It is difficult to quantify how long impaired performance is sustained after an uncivil incident, given the variation in behaviours, reactions and personalities involved. Given that our daily job requires intense focus as part of providing critical care, our undivided attention to technical skills, and large degree of engagement with our patients, this is concerning.
2. The observing team
The performance of all team members who witness incivility are affected by different mechanisms.
Studies have demonstrated that witnessing incivility significantly decrease one’s performance. A study published in 2013 showed that witnesses had a 20% reduction in performance and 50% decrease in willingness to help other members of their team.5
Good teams are built on foundations of mutual trust, cooperation, respect for each other, and commitment to achieving a mutual goal. How this gets disrupted when one is uncivil is significant. It not only breeds interpersonal conflicts, but in addition breaks down the teamwork and communication channels, which are critical in delivering high level care and performance.6 7
What is reported as being damaged, and in some cases even destroyed, is the ‘psychological safety’ of the team; impairing innovation, cessation of volunteering opinions and collective goals amongst members.8
3. The patient
The care provided to the patient is ultimately compromised, such as medical errors and delays in decision making.9
Rude language and hostile relationships between healthcare workers has been associated with serious threat to patient care, as well as a patient’s impressions of the care being delivered. The behaviour of the team member(s) can negatively impact the image of the care being delivered, and credibility of highly trained and skilled professionals can be impacted. This is accentuated by the patient often being in an anxious and sensitive emotional state, especially given they are undergoing clinical care in an environment surrounded by unfamiliar faces.
Some areas of medicine have performed controlled simulations to gauge the impact incivility has objectively. A randomised trial performed across 24 neonatal intensive care unit teams, involved an unwell infant and the treating team being exposed to rudeness or neutral comments. Unsurprisingly, results showed the team who was subject to incivility had lower scores in diagnostic (2.6 vs 3.2, p=0.005), and procedural performance (2.8 vs 3.3, p=0.008).10
A more recent study, published in 2019, examined anaesthetic trainee performance within a simulated surgical environment. The control group were exposed to a pleasant surgical environment, whereas the other group to a ‘rude’ environment. Trainees exposed to incivility had a significantly lower performance level, with 63.6% performing at a standard to achieve a pass level versus 91.2% within the control group (p=0.009).11
Although these examples are not strictly native to our specialty, we can empathise with these scenarios given their close relationship to clinical situations within obstetrics and gynaecology.
How can we change and become more civil?
Practice in self-care
It is important to take care of oneself, mentally, emotionally and physically. Self-care will result in positive mindfulness; and allow our body to rest, reflect and refocus in time.
Uncivil behaviour can directly and indirectly inflict negativity on ourselves; we lose our vision and our objectivity. We can feel depressed, anxious and stressed, as well as negatively reactive to what is occurring around us.12
By taking the time out for oneself, doing something of pleasure and refocusing, this is the best medicine for promoting civility amongst our workplaces.
Civility Saves Lives
This is a UK campaign that was devised initially by a small group of medical professionals who acted to raise awareness of the power of civility in medicine. Since then, Civility Saves Lives has grown into a large organisation that promotes positive behaviours internationally using social media campaigns, clear and powerful infographics, publications and international presentations.13
The message is strong. By being aware of our interactions with others and focusing on being civil, it will help reduce error, stress and complications in our clinical practice.
‘Civility costs nothing and buys everything’
– Lady Mary Wortley Montagu
To be civil is not expensive. Civility does not require years of medical and specialty school training. It can be taught without the use of textbooks and online resources, by any level of any professional.
Has the time come where we need to embed formal training in civility within our departments? Take a moment to look around you – observe the room, each individual and their interactions. Treat others as you wish to be treated. Say sorry. Ask for feedback at the time of encounters. Do things differently next time. None of this costs money.
Be a leader; to be civil is part of a leader’s true characteristics and will enhance not only your performance, but everyone around you.14
Although there are things left to be answered, it is time to put a stop to incivility. It can impose a toll on many individuals and our overall performance as a team, department, hospital and system. Let’s together in 2020 be proactive. Let’s recognise, address and say goodbye to incivility.
References
- Bradley V, Liddle S, Shaw R, et al. Sticks and stones: investigating rude, dismissive and aggressive communication between doctors. Clinical Medicine. 2015;15(6):541-545.
- Bradley V, Liddle S, Shaw R, et al. Sticks and stones: investigating rude, dismissive and aggressive communication between doctors. Clinical Medicine. 2015;15(6):541-545.
- Risk A, Erez A, Foulk TA, et al. The Impact of Rudeness on Medical Team Performance: A Randomized Trial. Pediatrics. 2015; 136(3):487-95.
- Katz D, Blasius K, Isaak R, et al. Exposure in incivility hinders clinical performance in a simulated operative crisis. BMJ Quality and Safety. 2019;28:750-7.
- Klingberg K, Gadelhak K, Jegerlehner SN, et al. Bad manners in the Emergency Department: Incivility among doctors. PLoS ONE. 2018;13(3):e0194933.
- Risk A, Erez A, Foulk TA, et al. The Impact of Rudeness on Medical Team Performance: A Randomized Trial. Pediatrics. 2015; 136(3):487-95.
- Katz D, Blasius K, Isaak R, et al. Exposure in incivility hinders clinical performance in a simulated operative crisis. BMJ Quality and Safety. 2019;28:750-7.
- Porath C, Pearson C. The price of incivility. Harvard Business Review. 2013;91:114-21.
- Katz D, Blasius K, Isaak R, et al. Exposure in incivility hinders clinical performance in a simulated operative crisis. BMJ Quality and Safety. 2019;28:750-7.
- Risk A, Erez A, Foulk TA, et al. The Impact of Rudeness on Medical Team Performance: A Randomized Trial. Pediatrics. 2015; 136(3):487-95.
- Katz D, Blasius K, Isaak R, et al. Exposure in incivility hinders clinical performance in a simulated operative crisis. BMJ Quality and Safety. 2019;28:750-7.
- Clark CM. Conversations to inspire and promote a more civil workplace: Let’s end the silence that surrounds civility. American Nurse Today. 2015;10(11):18-22.
- Civility Saves Lives. Available from: civilitysaveslives.com
- Katz D, Blasius K, Isaak R, et al. Exposure in incivility hinders clinical performance in a simulated operative crisis. BMJ Quality and Safety. 2019;28:750-7.




Great read Jess!