The formation of peritoneal adhesions following surgery is a common problem that can have significant implications both to the individual and to the healthcare system.
The need for effective adhesion prevention strategies has been extensively reported in the literature. This article provides a summary of the available evidence, as well as a practical guide towards better strategies for adhesion prevention.
Clinical significance
Adhesions may occur after both laparotomy and laparoscopy. Postoperative adhesions have been reported in 60–90% of women who underwent extensive open gynaecological surgery.1
Although often asymptomatic, adhesions can be associated with significant morbidity, including bowel obstruction (adhesions account for 30–41% of all cases of intestinal obstruction and 65–75% of small bowel instruction requiring further surgery),2 3 chronic pelvic pain, deep dyspareunia and female subfertility4 (up to 15–20% of infertility in women is secondary to adhesions).5
A Scottish study that followed 8489 women who underwent open gynaecological surgery showed that 34.5% were readmitted one or more times over the following 10 years because of adhesion-related complications. The highest rate of readmission (48%) was in women whose primary site of surgery was the ovary.6
In addition, adhesions may increase the risk of complications during subsequent surgery, including difficult surgical access, increased risk of injury to bowel and genitourinary tract, blood loss and increased duration of surgery.7 8 9
Pathophysiology
Adhesion formation is triggered by injury to the peritoneal mesothelium, which initiates a peritoneal repair response. Adhesions can develop within the first few hours after surgery, depending on the fine balance between pathways that promote fibrin deposition and others that cause degradation (fibrinolysis). Factors that favour the deposition of fibrin over its degradation will lead to the formation of fibrinous bridges between adjacent peritoneal surfaces. The two main factors associated with surgical injury that escalate the organisation of fibrin into adhesions are inflammation and tissue ischaemia.
At a biomolecular level, the injury to tissue triggers the release of cytokines, growth factors, cell adhesion molecules and histamine, mediators of the local inflammatory response that promote fibrin deposition. This inflammatory reaction involves processes such as coagulation and the recruitment of leucocytes (macrophages and neutrophils) and fibroblasts. In particular, macrophages are involved in the recruitment of adjacent mesothelial cells and fibroblasts, which migrate to the site of peritoneal injury and re-epithelialise the injured peritoneal surface over 3–5 days. Adhesion formation usually occurs within this 3–5-day window, which has clinical implications for the efficacy of anti-adhesion agents that must also be active over this period.
Tissue damage associated with ischaemia also promotes the formation of peritoneal adhesions as a maladaptive response. The response is an attempt to revascularise areas of relative ischaemia following surgical procedures such as ligation, fulguration or crushing, which disrupt tissue vasculature.
Lastly, contamination of the peritoneal cavity with materials such as sutures, talcum powder, starch, faeces or bacteria may induce further inflammation, which inhibits fibrinolysis and increases the likelihood of adhesion formation. Hence the importance of measures that reduce contamination.
Strategies to prevent adhesions
Adhesion-prevention strategies can be broadly categorised into injury minimisation via meticulous surgical technique and reduced tissue trauma, placing a physical barrier between peritoneal surfaces and the use of pharmacological agents to modulate the cellular response to tissue injury.10 11
Meticulous surgical technique / careful tissue handling
The treatment of adhesive disease is very difficult and most patients who undergo surgery for adhesiolysis develop adhesions to a similar degree. The best strategy is to avoid, as much as possible, initial adhesion formation. All measures that reduce epithelial damage should be routinely employed. Precise and meticulous surgical technique, which includes gentle handling of tissue and meticulous haemostasis, reduces adhesion formation.
The method of surgical approach is also important; laparoscopic techniques involve smaller incisions and reduced exposure to foreign materials leading to reduced injury. Nevertheless, adhesions can still occur depending on the type and extent of the surgery performed as well as individual patient characteristics. Copious irrigation is recommended to minimise contamination.
Adhesion barriers
Physical barriers aim to reduce the formation of fibrinous attachments between injured peritoneal surfaces by keeping them apart, particularly for the first 72 hours. Physical barrier agents in either solid or liquid forms have been developed and there is randomised trial data showing some evidence of benefit.
Figure 1 demonstrates the classification and types of physical barrier agents and Table 1 summarises the advantages and disadvantages of commonly used types.
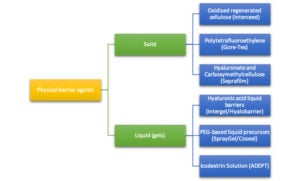
Figure 1. Classification of adhesion barriers.
Pharmacological agents
Corticosteroids have been considered as a way to prevent adhesions based on their anti-inflammatory properties. At present, there is no evidence to support their use. A meta-analysis of five RCTs that investigated the efficacy of steroids in preventing adhesions showed that neither adhesion formation nor pregnancy rates improved, with the potential for an increased risk of infection in the perioperative setting.12 Similarly, studies that used heparin to try to prevent adhesions have also not shown benefit, either alone or in combination with barrier methods.
Oophoropexy
Ovarian adhesions are a common consequence of surgery for the removal of ovarian cysts and, most importantly, surgery for the treatment of endometriosis. The main implications of ovarian adhesions are infertility and chronic pelvic pain. In addition to the several techniques described in this article, authors have proposed suspending the ovaries with the use of sutures to keep them away from the pelvic sidewalls during the first few days after endometriosis surgery.
A meta-analysis of several clinical trials published last year concluded that the procedure carries very low risk and was shown to be beneficial for adhesion prevention.13 The limitations of the review include the fact that it is a relatively new procedure (most studies included in the analysis were published after 2011), there were only two RCTs and the studies used different techniques for the oophoropexy (for example, permanent or absorbable sutures, intra or extra abdominal tying) and for the assessment of postoperative adhesion formation (transvaginal ultrasound, second look laparoscopy, etc).
Initial evidence suggests that ovarian suspension can be an effective strategy in preventing postoperative ovarian adhesion formation in women undergoing laparoscopic surgery for stage III–IV endometriosis. The authors have been doing this consistently with a quick absorption polyglactin 910 suture (2-0 vicryl rapide, Ethicon, US) used to suspend the ovaries to the ipsilateral round ligament whenever the surgery requires extensive dissection of the pelvic sidewalls or the removal of endometriomas.
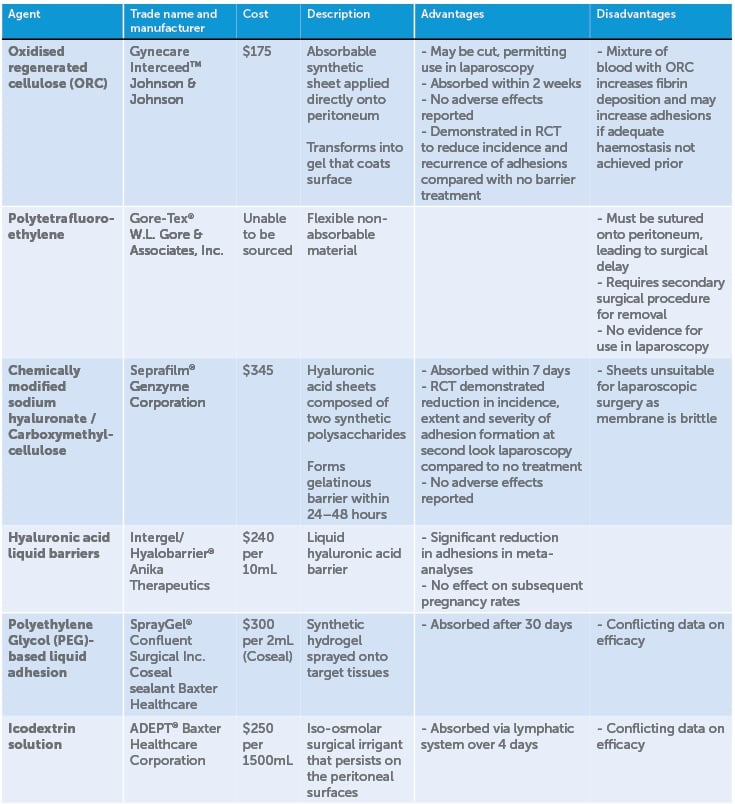
Table 1. Summary of adhesion barriers.
Conclusion
Postoperative adhesions are a significant source of patient morbidity and place a considerable burden on the health system. Aside from meticulous surgical technique, few agents have a solid evidence base of efficacy, with little long-term data on safety. Progress has been made in recent years, with some products showing some success in reducing adhesion formation. Much work and further research is still required to develop new products that can more effectively reduce the formation of surgical adhesions to improve clinical outcomes, reduce the health implications to individuals and the overall impact to the health system.
References
- Monk BJ, Berman ML, Montz FJ. Adhesions after extensive gynecologic surgery: clinical significance, etiology and prevention. Am J Obstet Gynecol. 1994;170:1396-1403.
- Menzies D. Postoperative adhesions: their treatment and relevance in clinical practice. Ann R Coll Surg Engl. 1993;75:147-53.
- Ellis H. The magnitude of adhesion related problems. Ann Chir Gynaecol. 1998;87:9-11.
- Robertson D, Lefebvre G. Adhesion prevention in gynaecological surgery. J Obstet Gynaecol Canada. 2010;32(6):598-602.
- Soules MR, Dennis L, Bosarge A, Moore DE. The prevention of postoperative pelvic adhesions: an animal study comparing barrier methods with dextran 70. Am J Obstet Gynecol. 1982;143:829-34.
- Lower AM, Hawthorn RJS, Ellis H, et al. The impact of adhesions on hospital readmissions over ten years after 8849 open gynaecological operations: an assessment from the Surgical and Clinical Adhesions Research study. BJOG. 2000;107:855-62.
- ten Broek RP, Schreinemacher MH, Jilesen AP, et al. Enterotomy risk in abdominal wall repair: a prospective study. Annals of Surgery. 2012;256(2):280-7.
- ten Broek RP, Strik C, Issa Y, et al. Adhesiolysis-related morbidity in abdominal surgery. Annals of Surgery. 2013;258(1):98-106.
- Van Der Krabben AA, Dijkstra FR, Nieuwenhuijzen M, et al Morbidity and mortality of inadvertent enterotomy during adhesiotomy. British Journal of Surgery. 2000;87(4):467-71.
- Diamond MP. Reduction of postoperative adhesion development. Fertil Steril. 2016;106(5):994-7.e1.
- Aref-Adib M, Phan T, Ades A. Preventing adhesions in laparoscopic surgery: the role of anti-adhesion agents. The Obstetrician and Gynaecologist. 2019;21(3):doi 10.1111/tog.12588.
- Metwally M, Watson A, Lilford R, Vandekerckhove P. Fluid and pharmacological agents for adhesion prevention after gynaecological surgery. Cochrane Database Syst Rev. 2006(2):Cd001298.
- Giampaolino P, Della Corte L, Saccone G, et al. Role of Ovarian Suspension in Preventing Postsurgical Ovarian Adhesions in Patients with Stage III-IV Pelvic Endometriosis: A Systematic Review. J Minim Invasive Gynecol. 2019;26(1)53-62.





Leave a Reply