Uterine rupture is defined as a full thickness separation of the uterine wall and the overlying serosa.1 It is associated with significant neonatal and maternal mortality and morbidity. It mainly occurs in third trimester;2 spontaneous uterine rupture in first trimester is rare and very difficult to diagnose.
Placenta accreta is abnormal placental implantation leading to an adherence of the placenta to the uterine wall.3 It is categorised according to degree of placental invasion into the uterine myometrium. The definition encompasses placenta accrete vera (adherence of the placenta to the superficial myometrium), placenta increta (adherence of the placenta to the body of the myometrium – but not the entire thickness) and the most catastrophic subtype, placenta percreta (penetration and adherence of the placenta through the full thickness of the myometrium, the uterine serosa and potentially nearby organs).4 The incidence of uterine rupture due to placenta percreta is rare at 1 in 5000 women;5 previous caesarean section delivery is the predominant risk factor. Here we present to you two concurrent rare occurrences, a case of uterine rupture in second trimester in the setting of placenta percreta.
Case
A 30-year-old woman presented at 20+1 weeks gestation, with post-coital exacerbation of generalised abdominal pain. She did not report vaginal bleeding.
She had had two previous lower segment caesarean sections at term overseas. The morphology scan at 19 weeks and 3 days reported an anterior placenta previa covering the cervical os by 5.1 cm.
On examination, the patient was diaphoretic and pale, with a blood pressure 78/53 and a heart rate 105. She had generalised abdominal tenderness with gross abdominal distension. Blood investigation revealed dropping haemoglobin levels (83 g/L to 61 g/L two hours apart), INR 1.3 and fibrinogen 1.8 mg/dL.
An urgent ultrasound reported large free fluid in the abdomen. The patient was immediately taken to theatre. Laparoscopic entry proved difficult visualisation as blood refluxed into the laparoscopic port and a four-quadrant hemoperitoneum obstructed visualisation of pelvic contents. A large round haemorrhagic mass was seen centrally and thought to be a haemorrhagic cyst (Figure 1).

Figure 1. View upon laparoscopic entry of a large central pelvic mass with areas of haemorrhage and prominent large surface vessels.
Decision for conversion to laparotomy through previous caesarean scar found placenta percreta with a ruptured lower uterine segment (Figures 2a and 2b). The central mass seen on laparoscopy was, in fact, the uterus with abruption and large surface vessels.
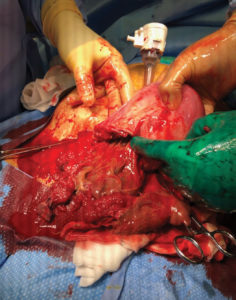
Figure 2a. Lower segment uterine rupture with an adherent placenta.
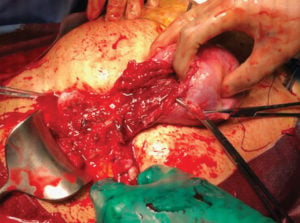
Figure 2b. Significant distortion of the lower uterine segment from uterine rupture.
The fetus was entirely expelled in the abdomen. Due to extensive uterine bleeding and distorted uterine anatomy, the decision was made for subtotal hysterectomy (Figure 3).
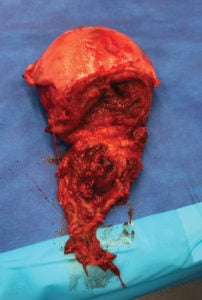
Figure 3. Subtotal hysterectomy specimen with adherent placental tissue.
Total blood loss was 4000 mL. The patient received 8 units of packed red blood cells, 7 bags of fresh frozen plasma, 1 unit of platelets and 3 L of crystalloid fluids; postoperative care was in ICU. She was discharged home on day six. The fetus weighed 250 g.
Histopathology confirmed placenta percreta with uterine rupture involving the anterior lower uterine segment and adjacent endocervix (Figure 4). β-hCG monitoring found a level of 1149 IU/L at presentation, and came down to less than 1 IU/L three weeks post discharge.
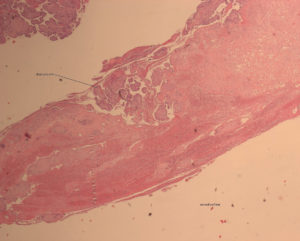
Figure 4. This histopathology slide demonstrates that two key elements of normal placental implantation are not present: there is no decidua between the chorionic villi and the uterus, and there is no myometrium. [H&E stain]. Image Courtesy of Liverpool Hospital Anatomical Pathology and A/Prof Leonardo Santos and Dr Miriam Fewtrell..
Discussion
In normal implantation, there is a layer of decidua that separates the placental villi from the myometrium at the area of implantation; in adherent placenta, this is lacking.6 Adherent placenta is rare, with incidence ranging from 1:500–1:93 000 deliveries.7 Placental accreta constitutes 78–80 per cent of cases, with placental increta and percreta constituting 15 per cent and 5–7 per cent of remaining cases of adherent placentation respectively.8 9 Placenta percreta is the most aggressive form of the spectrum, an obstetric complication that can have catastrophic consequences. In adherent placenta, the maternal mortality rate is 7–11.10 per cent and neonatal mortality is 9.76 per cent, with such rates mostly accredited to placenta percreta complications.
Previous caesarean section is the leading risk factor for uterine rupture as per the presented case. Other risk factors include fetal malpresentation, shoulder dystocia, neglected labour, breech extraction, instrumental-assisted vaginal delivery,11 previous uterine instrumentation, grand-multiparity and abnormal placentation.12 Abnormal placentation weakens the area of invasion in the myometrium, predisposing to uterine rupture.13 Jang et al describe a case of uterine rupture caused by placenta percreta in a patient with a history of dilation and curettage for a spontaneous miscarriage.14 There are case reports of abnormal placentation and spontaneous uterine rupture in first trimester in patients who underwent assisted reproduction. Norwitz et al15 report a case of uterine rupture after pelvic radiation causing abnormal placentation (calls upon good history-taking).
Placenta percreta-induced spontaneous uterine rupture more commonly occurs in the second and third trimesters; however, there have been rare cases where it has occurred between 10–20 weeks gestation.16 17 While the overall incidence of placenta percreta is low, increasing caesarean section rates in modern obstetrics is leading to increasing rates of placenta percreta.18 19 In women with placenta previa, the frequency of placenta accreta increases with increasing number of caesarean deliveries as per Silver RM et al.20 21
Clinical signs of uterine rupture include acute abdominal pain, scar tenderness, vaginal bleeding and maternal tachycardia and hypotension;22 however, some signs may not be present as our patient had insidious onset of abdominal pain and no vaginal bleeding. There is significant fetal and maternal morbidity and mortality in delayed diagnosis of uterine rupture. Potential complications include fetal death, maternal haemorrhage, injury to nearby organs, emergency hysterectomy and maternal death.23
Delayed diagnosis may be attributable to consideration of more common diagnoses, such as a ruptured ovarian cyst. As such, uterine rupture and placenta percreta should be considered in all pregnant women who present with an acute haemorrhagic abdomen at the start of pregnancy.
It is crucial to appreciate the roles of imaging and investigations to minimise morbidity and mortality and allow for early planning and potential conservative treatment.24 If an adherent placenta is suspected on ultrasound, consider alpha-fetoprotein level, which tends to be elevated, and an MRI for placental mapping when ultrasound findings are inconclusive.25 26
Diagnosis of adherent placenta using ultrasound in first trimester is challenging with a sensitivity of 41 per cent; however, ultrasonography in the first trimester should raise suspicion of an adherent placenta in a patient with prior caesarean section if it reveals a placenta previa. 75 per cent of placenta percreta cases are associated with previously known placenta praevias.27 28 29
There’s the question as to whether our patient with a previous caesarean section and a placenta previa on the morphology scan should have been urgently referred to a tertiary hospital for counselling on further management in light of the complications involved, with utilisation of fetomaternal unit assessment and MRI.
There’s the thought that if ultrasound at the morphology scan had questioned placenta percreta, our patient may have been sent in urgently to a tertiary centre to discuss continuation of pregnancy and prolonged hospital admission (with risk of prematurity) versus termination of pregnancy. This raises the question whether there was potential to pick up uterine rupture earlier and whether intercourse triggered the rupture due to further mechanical weakening.
There are reports of conservative treatment of placenta percreta-induced uterine rupture such as uterine curettage with packing, postoperative chemotherapy, and uterine artery occlusion.30 The four-fold mortality associated with conservative treatment in comparison to a hysterectomy, however, justifies an emergency hysterectomy to be the preferred approach.31
Conclusion
Diagnosis of adherent placenta in early pregnancy is a challenge. This case serves as a reminder to consider uterine rupture as a differential diagnosis in the acute abdomen in early pregnancy, and use of thorough clinical and investigative skills to derive a diagnosis. While a difficult decision, laparoscopy should be considered for investigation of undifferentiated acute abdomen in first trimester of pregnancy.32
Early suspicion for placenta praevia and percreta allows for further assessment with fetomaternal unit referral and consideration of MRI, as well as multidisciplinary team utilisation for delivery planning.
References
- UpToDate. Placenta previa: Epidemiology, clinical features, diagnosis, morbidity and mortality. 2019. Available from: www.uptodate.com/contents/placenta-previa-epidemiology-clinical-features-diagnosis-morbidity-and-mortality.
- Dahiya P, Nayar KD, Gulati AJ, Dahiya K. Placenta Accreta Causing Uterine Rupture in Second Trimester of Pregnancy after in vitro Fertilization: A Case Report. Journal of Reproduction & Infertility. 2012;13(1),61-3.
- Dahiya P, Nayar KD, Gulati AJ, Dahiya K. Placenta Accreta Causing Uterine Rupture in Second Trimester of Pregnancy after in vitro Fertilization: A Case Report. Journal of Reproduction & Infertility. 2012;13(1),61-3.
- Konijeti R, Rajfer J, Askari A. Placenta percreta and the urologist. Reviews in Urology. 2009;11(3),173-6.
- Jang DG, Lee GS, Yoon JH, Lee SJ. Placenta percreta-induced uterine rupture diagnosed by laparoscopy in the first trimester. International Journal of Medical Sciences. 2011;8(5):424-7.
- Konijeti R, Rajfer J, Askari A. Placenta percreta and the urologist. Reviews in Urology. 2009;11(3),173-6.
- Dahiya P, Nayar KD, Gulati AJ, Dahiya K. Placenta Accreta Causing Uterine Rupture in Second Trimester of Pregnancy after in vitro Fertilization: A Case Report. Journal of Reproduction & Infertility. 2012;13(1),61-3.
- Konijeti R, Rajfer J, Askari A. Placenta percreta and the urologist. Reviews in Urology. 2009;11(3),173-6.
- Jang DG, Lee GS, Yoon JH, Lee SJ. Placenta percreta-induced uterine rupture diagnosed by laparoscopy in the first trimester. International Journal of Medical Sciences. 2011;8(5):424-7.
- Jang DG, Lee GS, Yoon JH, Lee SJ. Placenta percreta-induced uterine rupture diagnosed by laparoscopy in the first trimester. International Journal of Medical Sciences. 2011;8(5):424-7.
- UpToDate. Placenta previa: Epidemiology, clinical features, diagnosis, morbidity and mortality. 2019. Available from: www.uptodate.com/contents/placenta-previa-epidemiology-clinical-features-diagnosis-morbidity-and-mortality.
- Dahiya P, Nayar KD, Gulati AJ, Dahiya K. Placenta Accreta Causing Uterine Rupture in Second Trimester of Pregnancy after in vitro Fertilization: A Case Report. Journal of Reproduction & Infertility. 2012;13(1),61-3.
- Dahiya P, Nayar KD, Gulati AJ, Dahiya K. Placenta Accreta Causing Uterine Rupture in Second Trimester of Pregnancy after in vitro Fertilization: A Case Report. Journal of Reproduction & Infertility. 2012;13(1),61-3.
- Jang DG, Lee GS, Yoon JH, Lee SJ. Placenta percreta-induced uterine rupture diagnosed by laparoscopy in the first trimester. International Journal of Medical Sciences. 2011;8(5):424-7.
- Norwitz E, Stern H, Grier H, Lee-Parritz A. Placenta Percreta and Uterine Rupture Associated with Prior Whole Body Radiation Therapy. Obstetrics & Gynaecology. 2001;98(5, Part 2):929-31.
- Dahiya P, Nayar KD, Gulati AJ, Dahiya K. Placenta Accreta Causing Uterine Rupture in Second Trimester of Pregnancy after in vitro Fertilization: A Case Report. Journal of Reproduction & Infertility. 2012;13(1),61-3.
- Jang DG, Lee GS, Yoon JH, Lee SJ. Placenta percreta-induced uterine rupture diagnosed by laparoscopy in the first trimester. International Journal of Medical Sciences. 2011;8(5):424-7.
- Dahiya P, Nayar KD, Gulati AJ, Dahiya K. Placenta Accreta Causing Uterine Rupture in Second Trimester of Pregnancy after in vitro Fertilization: A Case Report. Journal of Reproduction & Infertility. 2012;13(1),61-3.
- Konijeti R, Rajfer J, Askari A. Placenta percreta and the urologist. Reviews in Urology. 2009;11(3),173-6.
- UpToDate. Placenta previa: Epidemiology, clinical features, diagnosis, morbidity and mortality. 2019. Available from: www.uptodate.com/contents/placenta-previa-epidemiology-clinical-features-diagnosis-morbidity-and-mortality.
- Silver R, Landon M, Rouse D, et al. Maternal Morbidity Associated with Multiple Repeat Caesarean Deliveries. Obstetrics & Gynaecology. 2006;107(6):1226-32
- Norwitz E, Stern H, Grier H, Lee-Parritz A. Placenta Percreta and Uterine Rupture Associated with Prior Whole Body Radiation Therapy. Obstetrics & Gynaecology. 2001;98(5, Part 2):929-31.
- Norwitz E, Stern H, Grier H, Lee-Parritz A. Placenta Percreta and Uterine Rupture Associated with Prior Whole Body Radiation Therapy. Obstetrics & Gynaecology. 2001;98(5, Part 2):929-31.
- Dahiya P, Nayar KD, Gulati AJ, Dahiya K. Placenta Accreta Causing Uterine Rupture in Second Trimester of Pregnancy after in vitro Fertilization: A Case Report. Journal of Reproduction & Infertility. 2012;13(1),61-3.
- Dahiya P, Nayar KD, Gulati AJ, Dahiya K. Placenta Accreta Causing Uterine Rupture in Second Trimester of Pregnancy after in vitro Fertilization: A Case Report. Journal of Reproduction & Infertility. 2012;13(1),61-3.
- Silver R, Landon M, Rouse D, et al. Maternal Morbidity Associated with Multiple Repeat Caesarean Deliveries. Obstetrics & Gynaecology. 2006;107(6):1226-32
- UpToDate. Placenta previa: Epidemiology, clinical features, diagnosis, morbidity and mortality. 2019. Available from: www.uptodate.com/contents/placenta-previa-epidemiology-clinical-features-diagnosis-morbidity-and-mortality.
- Konijeti R, Rajfer J, Askari A. Placenta percreta and the urologist. Reviews in Urology. 2009;11(3),173-6.
- Silver R, Landon M, Rouse D, et al. Maternal Morbidity Associated with Multiple Repeat Caesarean Deliveries. Obstetrics & Gynaecology. 2006;107(6):1226-32.
- Jang DG, Lee GS, Yoon JH, Lee SJ. Placenta percreta-induced uterine rupture diagnosed by laparoscopy in the first trimester. International Journal of Medical Sciences. 2011;8(5):424-7.
- Jang DG, Lee GS, Yoon JH, Lee SJ. Placenta percreta-induced uterine rupture diagnosed by laparoscopy in the first trimester. International Journal of Medical Sciences. 2011;8(5):424-7.
- Jang DG, Lee GS, Yoon JH, Lee SJ. Placenta percreta-induced uterine rupture diagnosed by laparoscopy in the first trimester. International Journal of Medical Sciences. 2011;8(5):424-7.





Leave a Reply