Antenatal care is a vehicle for multiple interventions, including health education, recognition of risk factors and family planning counselling. Delayed access to antenatal care reduces opportunity for appropriate screening and management of risk factors resulting in poor maternal and fetal outcomes.1
About 65–71 per cent of pregnant women in developing countries receive at least one antenatal visit, while 47 per cent have more than four visits;2 only 17 per cent book early, compared to developed countries where only 2.8–16 per cent book after 20 weeks.3
In Papua New Guinea (PNG), only 44–53 per cent of births are supervised and 33–79 per cent of pregnant women receive some form of antenatal care. A study done in Madang province of PNG noted that 39 per cent of women with bad obstetric outcomes delayed initiation of antenatal care.4 Although 60–70 per cent of women who delivered at Port Moresby General Hospital (PMGH) in 2015 had attended more than four antenatal visits, the maternal mortality ratio was 95.3 per 100 000 live births, while the perinatal mortality rate was 25 per 1000 deliveries; it was 19.5/1000 for women who had antenatal care and 67/1000 for non-attendants. The HIV rate was 4.3 per cent among non-attendants who were tested during labour versus 1.85 per cent for the attendants. The reduction in vertical transmission of HIV among attendant women has halved since 2010, when ART medications became available in PNG, from 17.7 per cent in 2010 to 8.2 per cent in 2014, a further testimony for the value of antenatal services for PNG.5
In most developing nations, it is always a struggle to get women to book early for antenatal care for various reasons including health workers’ bad attitude, limited number of staff, poor accessibility to the antenatal clinics (distance and cost), unhappy experience during previous pregnancies and efforts to avoid multiple visits to the clinic.6 In spite of the value of antenatal care, the low rate of utilisation of facilities and the reasons for this is why this study was initiated.
Methodology
The definition of early ‘booking’ for antenatal care at the PMGH is first attendance at 20 weeks gestation or less in contrast to the WHO definition of booking before 12 weeks gestation. Between 7 February and 6 July 2017, 821 women who attended PMGH for their first antenatal visit were interviewed to identify the main factors influencing the timing of their initiation for antenatal care. Significant variables were examined by univariate analysis and multiple regression analysis with p-values less than 0.05 and odds ratios whose confidence intervals did not include 1 taken as significant.
Ethical clearance for this study was given by the University of PNG School of Medicine and Health Sciences Ethical Committee and the management of the PMGH.
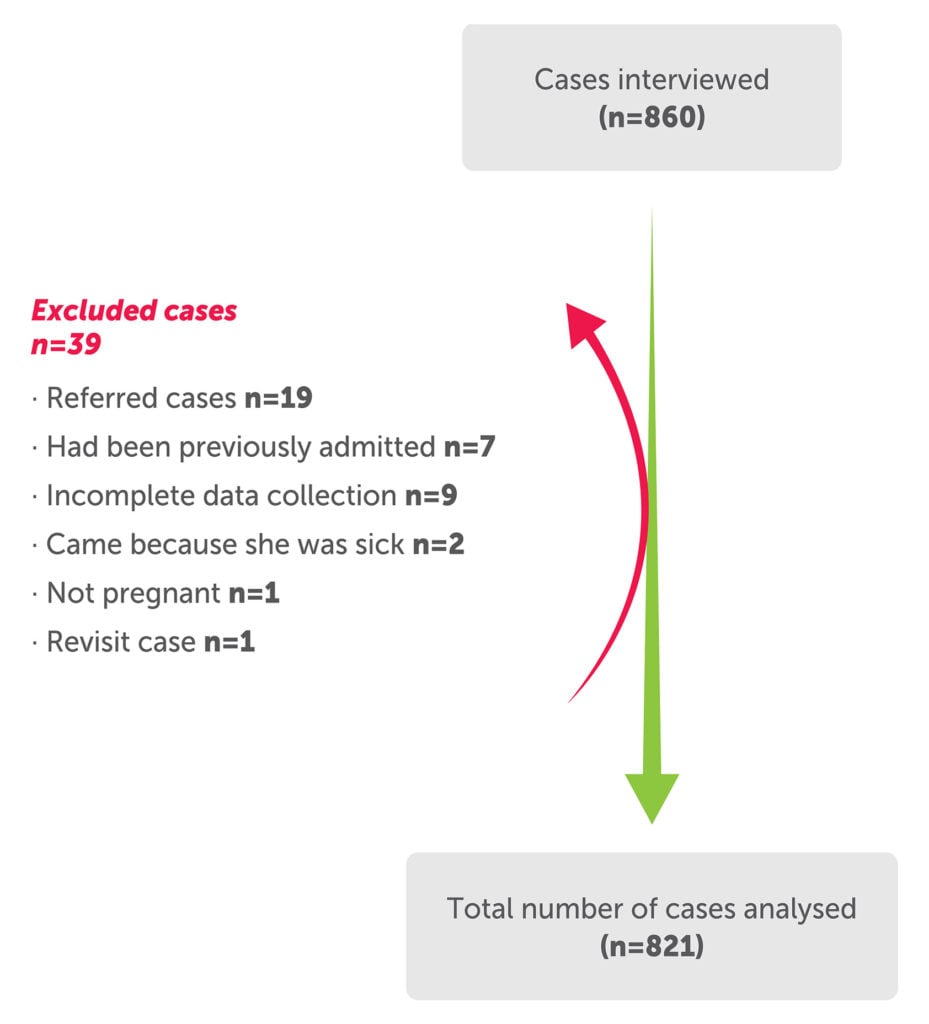
Figure 1. 860 cases interviewed with 39 excluded as per exclusion criteria.
Results
Using the PMGH definition of early booking, 81 per cent of the patients booked late for antenatal care. Figure 1 shows a total of 860 cases interviewed with 39 excluded as per exclusion criteria.
The mean age of women was 27 years, with a range of 15–45 years of age. Factors associated in univariate analysis with early antenatal booking, as highlighted in Table 1, included: primigravida, Highlands origin, previous bad obstetric history, previous family planning use, planning of this pregnancy, being happy with the pregnancy and those who perceived that it was the right time to initiate antenatal care. ‘Bad obstetric history’ included previous miscarriage, perinatal death, cardiac disease and ectopic pregnancy.
Factors associated with late booking included the following: no, or less than primary level, education of either the woman or her partner, patient’s low unemployment status, women living with an extended family, those avoiding frequent antenatal visits, those with other pressing obligations, hospital costs and those sent away at an earlier booking visit including women who came early but were told to return at quickening, as well as women who missed the ‘first 20 women to be enrolled’ cut.
The multiple regression analysis has noted significant variables in early booking (Table 2). It confirmed that women who were of Highlands origin, and those who perceived that it was the right time to book, those who were not unemployed and who did not avoid too many hospital visits were all likely to book early for antenatal care.
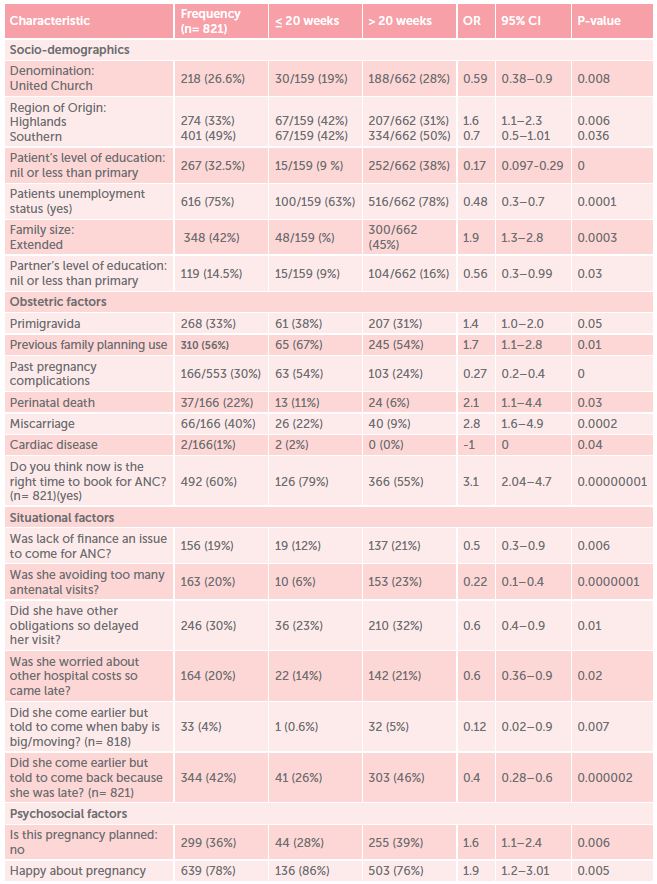
Table 1. Variables influencing initiation of antenatal booking using early booking as ≤ 20 weeks gestation.
Discussion
An analysis of 45 developing countries showed that 81–91 per cent of women start antenatal care late (that is, after 20 weeks) which is very similar to our findings.7
Many similar studies have suggested that maternal age, marital factors, religion, ethnicity, level of education and occupation of both partners do have an influence on the timing of antenatal care, while others dispute these findings.8,9,10
This study noted that Highlands’ women were more likely to book early while Southern women were likely to book later. Whether this finding was related to the location of PMGH in the Southern region and therefore had the disadvantage of increased numbers of village and slum dwellers of Southern origin to influence socio-economic factors is uncertain.
It is gratifying to note that women with prior history of ectopic pregnancy booked early. These women are usually counselled to do so at the PMGH.
| Variables | Odds Ratio | 95% | C.I. | Coefficient | S. E. | Z-statistic | P-value |
| Do you think now is the right time to book (Yes) | 3.1634 | 1.7784 | 5.627 | 1.1516 | 0.2938 | 3.9192 | 0.0001 |
| Highlands (yes) | 1.9058 | 1.1547 | 3.1456 | 0.6449 | 0.2557 | 2.5225 | 0.0117 |
| Patients unemployed (no) | 0.488 | 0.2702 | 0.8814 | -0.7175 | 0.3017 | -2.3786 | 0.0174 |
| Was she avoiding too many antenatal clinics (No) | 0.2314 | 0.0949 | 0.5642 | -1.4635 | 0.4547 | -3.2187 | 0.0013 |
Table 2. Multiple logistic regression analysis of variables that were significantly associated with early booking in univariate analysis.
The correct timing of initiation of antenatal care has been a concern in many studies.11,12 Of note is partners’ support playing an important role in maternal and child health. Women with better formal education, those with partners who are also better educated and with skilled occupations and are supportive were more likely to book early.
At PMGH, 33 per cent of maternal deaths have an underlying medical condition.13 Many of these medical conditions will not be diagnosed and treated unless women book early for antenatal care. In this study, women expressed the need for public health education. When women understand the importance of booking early for antenatal care, and do so, many advantages accrue, such as establishing the gestation as accurately as possible to set the scene for future decision-making. This is so important that in the developed world, early pregnancy units are available to encourage, and eventually reduce, revisits for the majority to pay more attention to high-risk pregnancies.
Acknowledgements
We would like to acknowledge the RANZCOG Foundation Global Health Research Scholarship for funding this project.
References
- Maternal mortality in PNG, stories beyond the numbers – WHO/NDOH
- Centenary G. Factors influencing the utilization of late antenatal care services in rural areas. A case study of Kisoro district (Master’s thesis). 2001. Available from: http://makir.mak.ac.ug/bitstream/handle/10570/2031/Centenary%20Gloria%20Dissertation.pdf?sequence=1&isAllowed=y
- Villar J, Ba’aqueel H, Piaggio G, et al. WHO antenatal care randomised trial for the evaluation of a new model of routine antenatal care. Lancet. 2001;357(9268):1551-64.
- Andrew EVW, Pell C, Angwin A, et al. Factors affecting attendance at and timing of formal antenatal care; Results from a qualitative study in Madang, Papua New Guinea. PLoS ONE. 2014;9(5):e93025.
- Annual Hospital Statistics for Port Moresby General Hospital, 2015.
- Maternal mortality in PNG, stories beyond the numbers – WHO/NDOH
- Gudayu TW. Proportion and factors associated with late antenatal care booking among pregnant women in Gondar Town, North West, Ethiopia. African Journal of Reproductive Health. 2015;19(2):94-100.
- Banda I, Michelo C, Hazemba A. Factors associated with late antenatal care attendance in selected rural and rrban communities of the copperbelt province of Zambia. Medical Journal of Zambia. 2012;39:29-36.
- Gross K, Alba S, Glass TR, et al. Timing of antenatal care for adolescent and adult pregnant women in south-eastern Tanzania. BMC Pregnancy & Childbirth. 2012;12:16.
- Cresswell JA, Yu G, Hatherall B, et al. Predictors of the timing of initiation of antenatal care in an ethically diverse urban cohort in the UK. BMC Pregnancy & Childbirth. 2013;13:103.
- Gudayu TW. Proportion and factors associated with late antenatal care booking among pregnant women in Gondar Town, North West, Ethiopia. African Journal of Reproductive Health. 2015;19(2):94-100.
- Gross K, Alba S, Glass TR, et al. Timing of antenatal care for adolescent and adult pregnant women in south-eastern Tanzania. BMC Pregnancy & Childbirth. 2012;12:16.
- Annual Hospital Statistics for Port Moresby General Hospital, 2015.





Leave a Reply