Ergonomics is the study of a person’s efficiency and safety in their working environment. It is the way we design and use equipment to optimise performance. This article will review how the layout of equipment in theatre and common errors in surgical posture can contribute to the development of musculoskeletal symptoms or injury, as well as ways to avoid this.
Scope of the problem
Musculoskeletal symptoms are a prevalent issue for the gynaecology surgeon. A Canadian web-based survey of 495 O&G practitioners demonstrated high rates of lower back (75.6 per cent), neck (72.9 per cent), shoulder (66.6 per cent), upper back (61.6 per cent) and wrist/hand (60.9 per cent) pain1 within the preceding 12 months. Rates were higher in women than men, with an approximately two-fold odds ratio, which is in keeping with evidence from other studies. Many respondents felt that surgery caused or exacerbated their symptoms, yet these symptoms are often ignored. Other risk factors include volume of surgical cases,2 surgeon inexperience and lack of awareness of ergonomic principles.2
Laparoscopic surgery poses its own unique set of challenges to surgeon safety, owing to factors such as the relative static nature of surgeon posture, difficult operating position, potential for prolonged surgical time and the use of hand-help operating tools that require great precision of movement.3 In addition to musculoskeletal discomfort or injury, laparoscopic surgeons may experience ocular strain as well as mental stress and fatigue. The effect of these symptoms on surgeon health, performance and productivity may also have a wider reaching adverse effect on quality of patient care and efficiency of the healthcare system.
Intra-operative considerations
Equipment
It is important to consider the arrangement of the relatively large amount of equipment required in theatre for a laparoscopic case. Appropriate use provides space for the surgeon to move freely, without having to adopt an awkward posture or use extremes of range of movement to accommodate or use equipment.
Surgeon posture
Common errors in surgeon posture, which may also contribute to discomfort and injury, include forward head position, shoulder elevation and asymmetry in weight bearing.4 A forward head posture increases the relative weight of the head on the cervical spine and can lead to degenerative changes.
Strategies for improving posture include:
- Tucking in both arms of the patient (which needs to be negotiated to accommodate anaesthetic needs). This creates more operating space for the surgeon, allowing a more comfortable posture to be adopted.
- Developing a routine of regularly resetting posture, shifting position and performing stretches during longer cases to reduce lactic acid build-up in the muscles and load on the musculoskeletal system.
Table 1. Optimal arrangement and use of equipment in theatre.
| Equipment | Optimal use/position | Effect |
| Monitor/screen (see photos) |
|
|
| Surgical bed |
|
|
Electrosurgery equipment:
|
|
|
| Gel foot pads | Gel pad positioned underfoot. | Can help to reduce discomfort in the back, neck and feet with prolonged periods of standing. |
| Surgical bean bag | Securely positioned and activated underneath patient, especially in cases of elevated body mass index. | The resultant reduction in table width (in comparison to bed extensions) reduces the truncal abduction required to reach the patient. Also prevents the patient from sliding on the table while in Trendelenburg. |
| Surgical instruments | Select the appropriate tool and use the instrument only for the purpose for which it was designed. For example:
|
Correct instrument usage results in:
|
x
Education and training
A 2013 literature review, conducted by the Urogynaecology Department of the Harvard Medical School, demonstrated a significant lack of awareness of ergonomic principles by surgeons. In response to these findings, they created an accessible educational video to demonstrate these principles.12 (This can be accessed via YouTube). This type of educational resource should form part of initial surgical skills training for trainees, as well being referred to regularly by experienced surgeons.
RANZCOG laparoscopic simulation courses are run four times per year in New Zealand and are fully funded for trainees. These courses include in-theatre practical teaching on how to optimise the surgical environment, as well as exercises using lapsim computers and training boxes. Laparoscopic surgeons have to undergo a steep learning curve as we deal with unique physical and cognitive challenges. These include factors such as learning to accommodate for the fulcrum effect of instruments, the reduction in haptic feedback, the smaller degree of freedom in movements and the translation of two-dimensional images. These factors can result in poorer performance and significantly higher mental stress – both of which can be improved with the use of simulation training.
As well as education and simulation, physical fitness may have a role to play on the development of physical symptoms during laparoscopic surgery. For example, Tse et al13 described a trunk endurance training program resulting in a reduction in discomfort and error rate during a laparoscopic simulated task. If injury does occur, surgeons may need to use analgesics, physiotherapy, reduce their surgical workload or take sick leave to cope with musculoskeletal symptoms related to operating.14
Conclusion
Ergonomics includes the ongoing search for technology that alleviates these challenges. Easier activation energy devices, light and camera sources may become more readily available, such as voice-activated equipment and flat foot controls that employ rotation for activation.
But for now, remember:
- Head back, shoulders down and a balanced posture.
- Re-set or stretch in longer cases.
- Take a few extra moments for theatre setup.
- These measures could improve your quality of life and longevity as a laparoscopic surgeon.
 Figure 1. Good posture, neutral spine position, relaxed shoulders, easy access to foot pedal. |
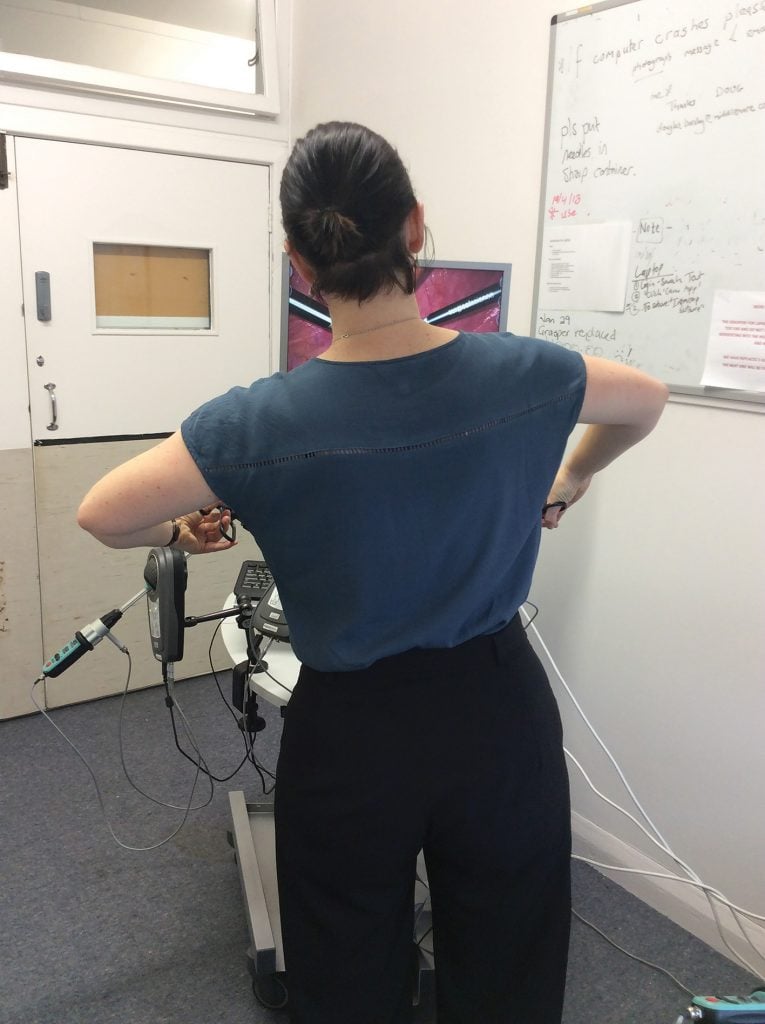 Figure 2. Poor posture with angle of spine, loading left hip, abducted arms. |
 Figure 3. Monitor in suboptimal position, resulting |
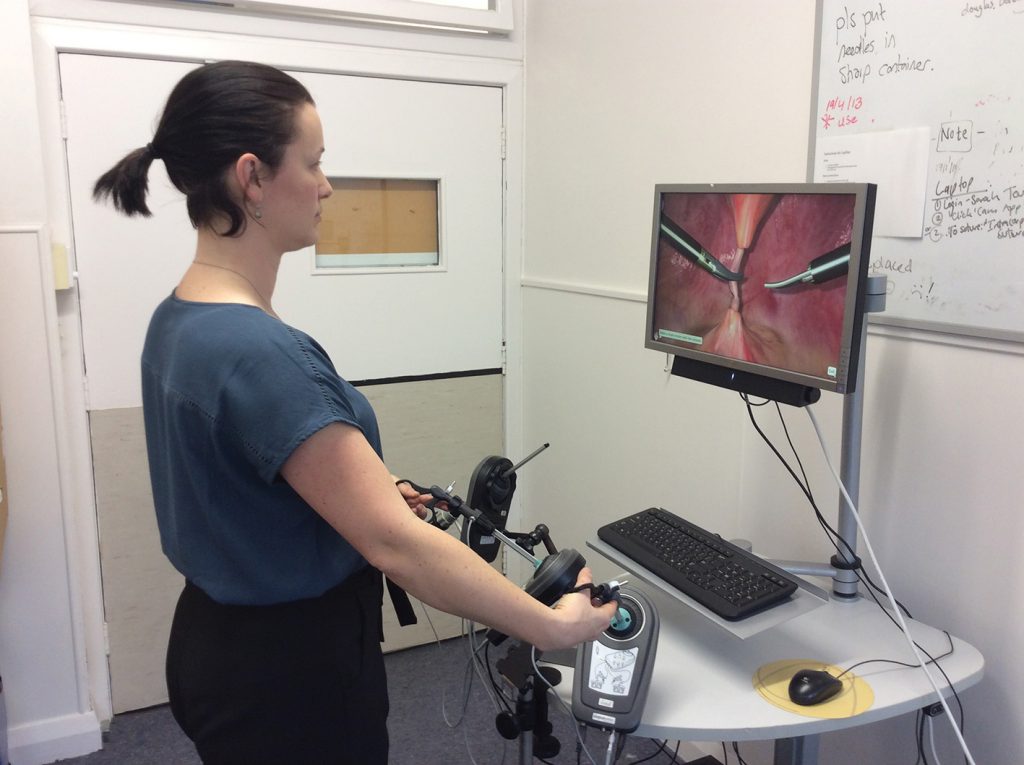 Figure 4. More comfortable head position with slight downward angle of gaze. |
References
- SR Adams, MR Hacker, JL McKinney, et al. Musckuloskeletal Pain in Gynecologic Surgeons. J Minim Invasive Gynecol. 2013;20(5)10.
- SR Adams, MR Hacker, JL McKinney, et al. Musckuloskeletal Pain in Gynecologic Surgeons. J Minim Invasive Gynecol. 2013;20(5)10.
- SD Choi. A review of the Ergonomic Issues in the Laparoscopic Operating Room. Journal of Healthcare Engineering. 2012;3(4):587-603.
- PL Rosenblatt, J McKinney, SR Adams. Ergonomics in the operating room: Protecting the surgeon. J Minim Invasive Gynecol. 2013;20(6):744.
- PL Rosenblatt, J McKinney, SR Adams. Ergonomics in the operating room: Protecting the surgeon. J Minim Invasive Gynecol. 2013;20(6):744.
- D Quinn, J Moohan. Optimal laparoscopic ergonomics in gynaecology. The Obstetrician & Gynaecologist. 2015;17:77-82.
- PL Rosenblatt, J McKinney, SR Adams. Ergonomics in the operating room: Protecting the surgeon. J Minim Invasive Gynecol. 2013;20(6):744.
- SD Choi. A review of the Ergonomic Issues in the Laparoscopic Operating Room. Journal of Healthcare Engineering. 2012;3(4):587-603.
- D Quinn, J Moohan. Optimal laparoscopic ergonomics in gynaecology. The Obstetrician & Gynaecologist. 2015;17:77-82.
- PL Rosenblatt, J McKinney, SR Adams. Ergonomics in the operating room: Protecting the surgeon. J Minim Invasive Gynecol. 2013;20(6):744.
- D Quinn, J Moohan. Optimal laparoscopic ergonomics in gynaecology. The Obstetrician & Gynaecologist. 2015;17:77-82.
- PL Rosenblatt, J McKinney, SR Adams. Ergonomics in the operating room: Protecting the surgeon. J Minim Invasive Gynecol. 2013;20(6):744.
- MA Tse, RS Masters, AM McManus, et al. Trunk muscle training, posture fatigue, and performance in laparoscopic surgery.
J Endourol. 2008;22:1053-8. - D Quinn, J Moohan. Optimal laparoscopic ergonomics in gynaecology. The Obstetrician & Gynaecologist. 2015;17:77-82.






Leave a Reply