For the broader O&G Magazine readership, balanced answers to those curly-yet-common questions in obstetrics and gynaecology.
Should we give antenatal corticosteroids to women with diabetes prior to planned late preterm delivery?
Diabetes mellitus in pregnancy, both pre-gestational and gestational, is increasingly common, and late preterm birth among these women is more common than in the general population. Antenatal corticosteroids are of clear benefit prior to preterm birth, but carry potential risks to mother and neonate in the presence of diabetes. As with any intervention in pregnancy, the balance of these benefits and risks must be considered prior to a decision to prescribe this therapy.
What are the benefits of antenatal corticosteroids?
Antenatal corticosteroid administration has been known to benefit the preterm infant since the sentinel trial of Liggins and Howie was reported in 1972.1 These initial observations have been conclusively replicated, with significant reductions in respiratory distress syndrome (RR 0.76), requirement for ventilatory support (RR 0.68), intraventricular haemorrhage (RR 0.55), necrotising enterocolitis (RR 0.50), and neonatal mortality (RR 0.69), in preterm neonates who receive a single course of corticosteroids.2 While initial studies demonstrated benefit for infants born before 34–35 weeks’ gestation, more recently, the Antenatal Late Preterm Steroids (ALPS) trial showed further benefit even up to 37 weeks, with a 20 per cent reduction in the requirement for respiratory support compared to placebo.3 4 One case of severe respiratory distress can be prevented for each 58 women given corticosteroids prior to late preterm birth.
What are the risks of antenatal corticosteroids?
In high-resource settings, corticosteroid administration in otherwise uncomplicated pregnancies confers benefit without apparent risk at gestations up to 34 weeks.5 However, neonatal hypoglycaemia has been reported in infants exposed to antenatal corticosteroids in the late preterm period,6 likely related to transient steroid-induced maternal hyperglycaemia with compensatory fetal hyperinsulinaemia, in line with the Pedersen hypothesis.7 This is generally mild and not associated with a prolonged hospital stay beyond what is normally required for a late preterm neonate.8
In women with diabetes, however, corticosteroid administration is not without risk for the mother or neonate. The glucocorticoid activity of steroid preparations at high doses can precipitate diabetic ketoacidosis in women with all forms of diabetes mellitus, if careful attention to hyperglycaemia and insulin therapy is not paid.9 Also, the maternal-fetal hyperglycaemia provoked by steroid administration just prior to birth may increase the incidence of neonatal hypoglycaemia and respiratory distress.10 11
What is the effect of diabetes on neonatal respiratory outcomes?
Infants of women with diabetes are at greater risk of severe neonatal respiratory distress syndrome compared to those of normoglycaemic mothers.12 Hyperinsulinaemia, as seen in maternal-fetal hyperglycaemia, directly impairs surfactant production and is likely to be a significant mechanism underlying respiratory distress in infants of diabetic mothers.13 Pre-labour caesarean section is more commonly required in the setting of diabetes, and is associated with a doubling in neonatal respiratory distress among late preterm infants independent of other contributors.14
What is the role for antenatal corticosteroid use in women with diabetes prior to late preterm birth?
To date, there has been no randomised trial of antenatal corticosteroids in this setting. A reduction in neonatal respiratory distress may be inferred from the results of studies such as ALPS, given the high risk of the outcome in this group, but women with pre-gestational diabetes were excluded from this and other trials due to concerns of potential adverse effects. Corticosteroids can have conflicting physiological effects in infants of women with diabetes, with the potential that beneficial effects on surfactant production could be outweighed by the suppressive influence of hyperinsulinaemia in steroid-induced hyperglycaemia (see Figure 1).
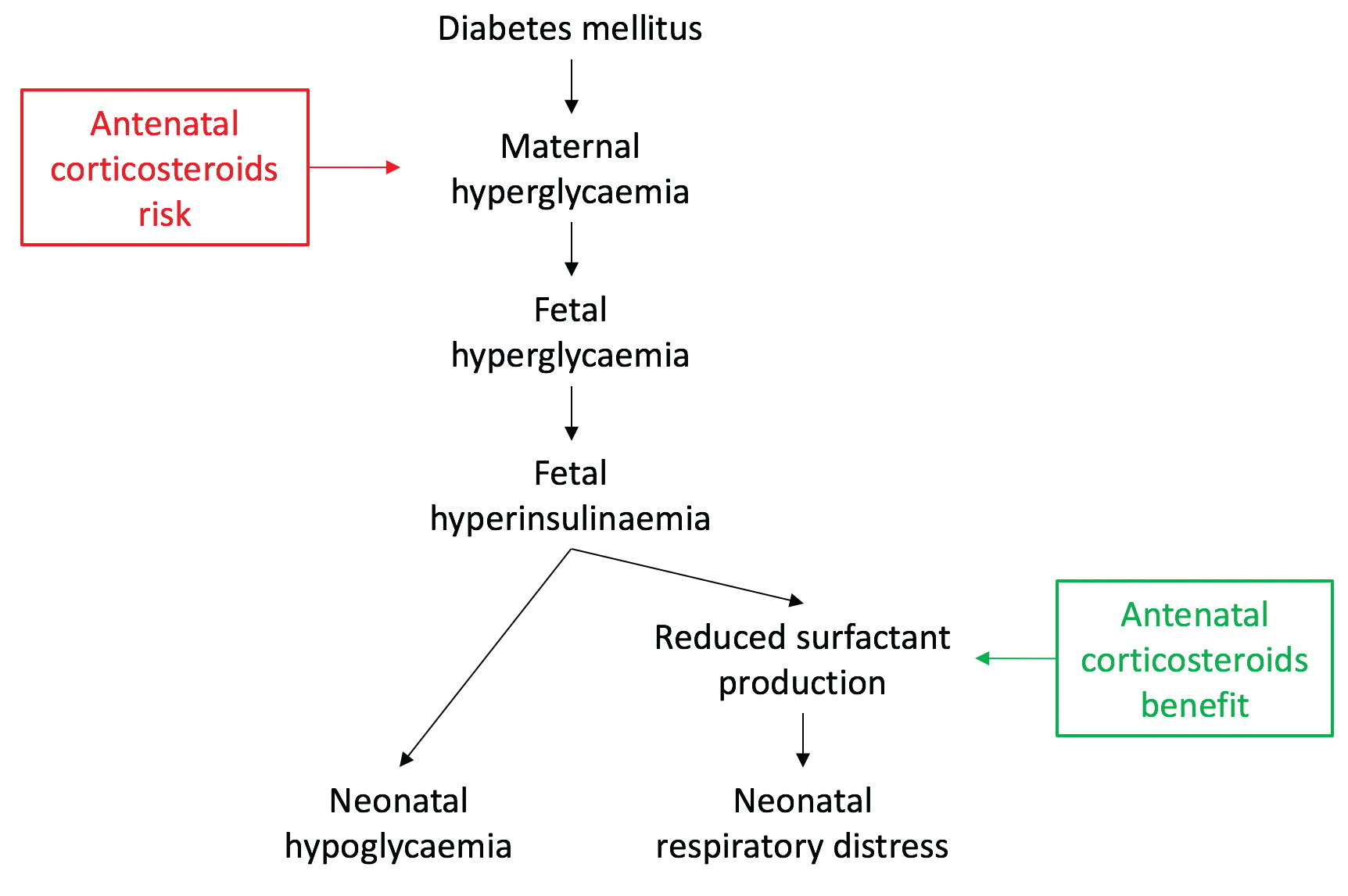
Figure 1. Mechanism of neonatal respiratory distress and hypoglycaemia in diabetes in pregnancy and the potential benefits and harms of antenatal corticosteroids.
Future studies will examine the role of antenatal corticosteroids in specific circumstances, such as prior to elective caesarean delivery, as well as the dose and route of steroid administration. In women with diabetes who are given corticosteroids, optimal post-steroid insulin management is still to be determined.
In the interim, in the absence of specific evidence to guide clinical practice, clinicians must consider the individual characteristics of each woman and fetus, such as gestation, quality of glycaemic control, planned mode of birth, and the risk of maternal complications in their prescribing decisions.
References
- Liggins GC, Howie RN. A controlled trial of antepartum glucocorticoid treatment for prevention of the respiratory distress syndrome in premature infants. Pediatrics 1972;50(4):515-25.
- Roberts D, Brown J, Medley N, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. The Cochrane Database of Systematic Reviews. 2017;3:Cd004454.
- Gyamfi-Bannerman C, Thom EA, Blackwell SC, Tita ATN, Reddy UM, Saade GR, et al. Antenatal betamethasone for women at risk for late preterm delivery. NEJM 2016;374(14):1311-20.
- Saccone G, Berghella V. Antenatal corticosteroids for maturity of term or near term fetuses: systematic review and meta-analysis of randomized controlled trials. BMJ 2016;355.
- Liggins GC, Howie RN. A controlled trial of antepartum glucocorticoid treatment for prevention of the respiratory distress syndrome in premature infants. Pediatrics 1972;50(4):515-25.
- Gyamfi-Bannerman C, Thom EA, Blackwell SC, Tita ATN, Reddy UM, Saade GR, et al. Antenatal betamethasone for women at risk for late preterm delivery. NEJM 2016;374(14):1311-20.
- Pedersen J. Diabetes and pregnancy: blood sugar or newborn infants [PhD thesis]. 1952, Copenhagen (Denmark), Danish Science Press.
- Gyamfi-Bannerman C, Thom EA, Blackwell SC, Tita ATN, Reddy UM, Saade GR, et al. Antenatal betamethasone for women at risk for late preterm delivery. NEJM 2016;374(14):1311-20.
- Bedalov A, Balasubramanyam A. Glucocorticoid-induced ketoacidosis in gestational diabetes: sequel of the acute treatment of preterm labor. Diab Care 1997;20(6):922-4.
- Gyamfi-Bannerman C, Thom EA, Blackwell SC, Tita ATN, Reddy UM, Saade GR, et al. Antenatal betamethasone for women at risk for late preterm delivery. NEJM 2016;374(14):1311-20.
- Piper JM, Xenakis EM, Langer O. Delayed appearance of pulmonary maturation markers is associated with poor glucose control in diabetic pregnancies. J Matern Fetal Med 1998;7(3):148-53.
- Mortier I, Blanc J, Tosello B, Gire C, Bretelle F, Carcopino X. Is gestational diabetes an independent risk factor or neonatal severe respiratory distress syndrome after 34 weeks of gestation? A prospective study. Arch Gynecol Obstet 2017;296(6):1071-7.
- Stubbs WA, Stubbs SM. Hyperinsulinism, diabetes mellitus, and respiratory distress of the newborn: a common link? Lancet 1978;1(8059):308-9.
- Indraccolo U, Pace M, Corona G, Bonito M, Indraccolo SR, Di Iorio R. Cesarean section in the absence of labor an d risk of respiratory complication in newborns: a case-control study. J Matern Fetal Neonatal Med 2017;1-7. doi: 10.1080/147670528.2017.1401999 [Epub].





Leave a Reply