Domestic violence and abuse against women is a global public health issue; it is embedded in society and pervades all socio-economic, gender and cultural groups, having a devastating effect on the lives of survivors.1 In most situations, domestic violence occurs within the context of a relationship of a cohabiting couple and includes physical, sexual and emotional abuse, as well as controlling behaviours. Indisputably, experiencing domestic violence and abuse can lead to negative consequences in many spheres of life, including educational achievement and economic opportunities, increased uptake of risky health behaviours and reduced capacity to parent.1
The nature of domestic violence
Domestic violence is a broad concept that affects the health and wellbeing of women, young girls and children.2 It can lead to severe injury, disability and death, as well as indirect health consequences; for example, psychological disorders such as post-traumatic stress disorder, depression, sleep disorders, suicide, social withdrawal and eating disorders, self-harm and substance abuse. In comparison to non-abused women, those in abusive relationships report higher rates of sexually transmitted infections, including HIV, as well as unintended pregnancies, repeated abortions and gynaecological problems.3 4 5
Domestic violence during pregnancy
Experiencing domestic violence at any time in a woman’s life can result in a multitude of harmful health problems. However, domestic violence during pregnancy should be of special concern as the violence not only poses a threat to the woman, but also to her unborn fetus. It is associated with placental abruption, premature rupture of membranes, premature birth, low birthweight, postnatal depression and maternal and perinatal death.6 The high rates of domestic violence and its known detrimental effects has resulted in health policy developments in many countries, including the UK, USA, Canada and Australia, where screening for domestic violence during and following pregnancy is endorsed.
Current debate around the effectiveness of routine enquiry for domestic violence
Those experiencing domestic violence are much more likely to seek healthcare than those who are not.7 However, engaging healthcare professionals in supporting women experiencing domestic violence has proved to be a challenge. Indeed, until very recently, health services have focused their energy and resources on dealing with the consequences of domestic violence.8 Proactive identification within healthcare settings and among health professionals has been poor for a variety of reasons, such as believing that domestic violence enquiry is not within their professional remit, fear of offending the woman, anxiety and nervousness about dealing with a positive disclosure and, most of all, a lack of training and education. In contrast, women experiencing domestic abuse consistently identify healthcare professionals as a potential source of support.9 10 Yet, unless women are asked directly about a history of violence, they are reluctant to disclose for fear of not being believed, being judged and stigmatised, having their children removed, or simply because they think nothing useful can be done about their situation.11
Conducting routine enquiry for domestic violence in all healthcare settings is keenly contested and several systematic reviews indicate that while there is evidence that screening increases identification, there is limited evidence to date that it increases referrals, reduces abuse or improves women’s health or safety.12 13 14 15 However, perhaps when assessing the effectiveness of interventions for women experiencing domestic violence, intermediate primary outcomes such as disclosure, validation of their experience and increased safety planning discussions may be more achievable and may even be a more meaningful measure than trying to measure an overall reduction in abuse.
What do women find helpful from health professionals?
Women who experience domestic violence will frequently access health services as they seek help for their injuries. In response, many professional health organisations have issued clinical guidelines on how to identify and respond appropriately to women and children have or are experiencing domestic violence and abuse.16 As mentioned previously, women find routine enquiry in certain health settings acceptable, providing that the health professional is caring, sensitive and non-judgemental. They want their experiences of violence to be believed and validated. It is important to acknowledge that routine enquiry for domestic violence may not be appropriate in all health settings, but maternity and women’s health services provide an ideal setting to communicate with women who are experiencing domestic violence. Though, to be able to do this safely and effectively, it is essential that healthcare professionals receive specialist education to be able ask the question in a sensitive manner and to be able to respond appropriately to a disclosure from a woman. Healthcare professionals must be educated and supported to provide appropriate and accurate advice and help to women and children. It is important that they are aware of their professional responsibilities and be familiar with appropriate referral pathways, while acknowledging the limitations of their role. (Table 1)
Routine enquiry for domestic violence and abuse can reach many women who previously have not been provided with an opportunity to disclose their history of violence. Most importantly, a visible healthcare response will not only promote disclosures of violence from women, but also communicate a strong message to society; that domestic violence and abuse in any form is no longer acceptable.17
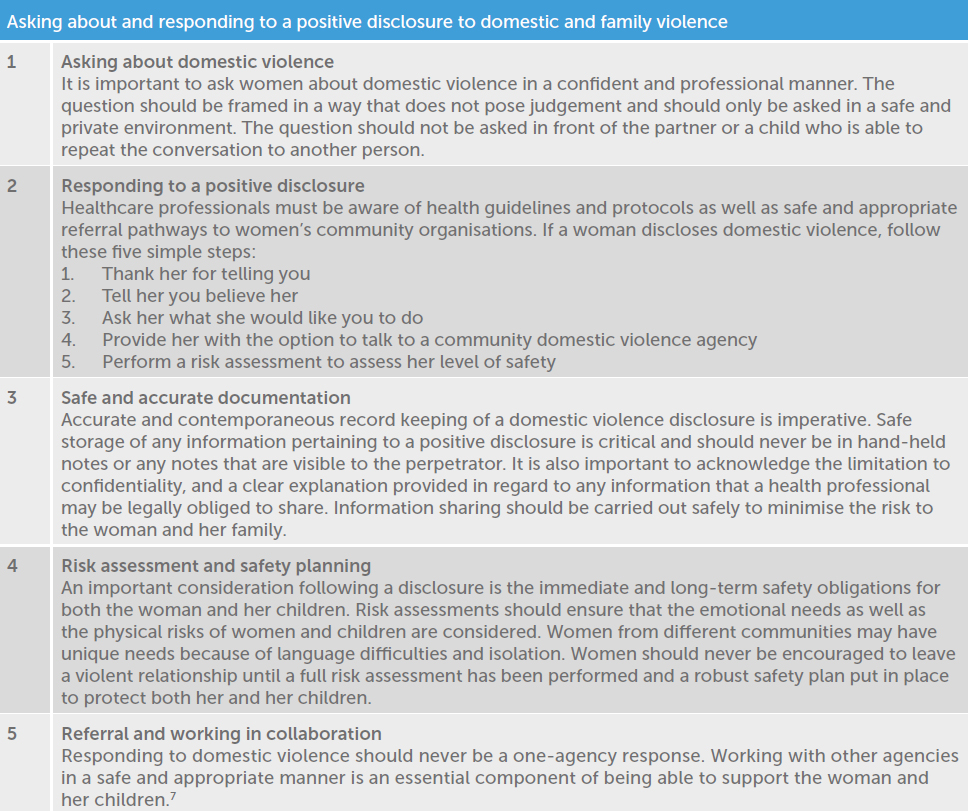
Table 1. Five simple steps to assist healthcare professionals to ask about domestic and family violence and respond appropriately.
Key messages
- The healthcare system has a significant role to play in a multisectoral response to violence against women
- A supportive response could be the catalyst to safety and recovery for women and children experiencing domestic violence
- All women disclosing domestic violence should be reassured that their information will be shared in a safe and appropriate manner
- All health organisations should have robust domestic violence policies and guidelines.
- Health services should provide support and ongoing domestic violence education
and training - Healthcare professionals who provide care
to women and children should be aware of local support agencies and the services they can provide - Routine enquiry/screening in this article refers to asking all adult women a set of standardised questions about a history of domestic violence at nominated health services such as maternity, mental health, drug and alcohol services, accident and emergency departments, sexual assault services and well women clinics, including gynaecology.
Domestic Violence Helpline
1800 RESPECT – 1800 737 732 (Australia) 24 hours, 7 days a week.
The AMA and Law Council of Victoria have developed Supporting Patients Experiencing Family Violence: a resource for medical practitioners, available here: ama.com.au/article/ama-family-violence-resource.
References
- World Health Organization. Responding to Intimate Partner Violence and Sexual Violence Against Women: WHO Clinical and Policy Guidelines. 2013. World Health Organization, Geneva.
- Baird K, T Mitchell. Using feminist phenomenology to explore women’s experiences of domestic violence in pregnancy. Br J Midwifery. 2014;22(6):418-26.
- Garcia-Moreno C, Pallitto C, Devries K, et al. Global and Regional Estimates of Violence against Women: Prevalence and Health Effects of intimate Partner Violence and Non-Partner Sexual Violence. 2013. World Health Organization, Geneva.
- Baird K, Creedy D, Mitchell T. Intimate partner violence and pregnancy intentions: a qualitative Study. J Clin Nurs. 2017;26:(15-6):2399-408.
- Taft AJ, Watson LF. Termination of pregnancy: associations with partner violence and other factors in a national cohort of young Australian women. Aust NZ J Public Health. 2007;31(2):135-42.
- Alhusen JL, Ray E, Sharps P, et al, Intimate partner violence during pregnancy: maternal and neonatal outcomes. J Womens Health. 2015;1:100-6.
- World Health Organization. Responding to Intimate Partner Violence and Sexual Violence Against Women: WHO Clinical and Policy Guidelines. 2013. World Health Organization, Geneva.
- Baird K, Gamble J. Domestic violence: midwives can make a difference. Australian Midwifery News. 2015;16(1)15-8.
- Baird K, Gamble J. Domestic violence: midwives can make a difference. Australian Midwifery News. 2015;16(1)15-8.
- Baird K, Salmon D, White P. A five year follow-up study of the Bristol pregnancy domestic violence programme to promote routine enquiry. Midwifery. 2013;29:1003-10.
- Baird K, Gamble J. Domestic violence: midwives can make a difference. Australian Midwifery News. 2015;16(1)15-8.
- Ramsay J, Richardson J, Carter Y, et al, Should health professionals screen women for domestic violence? Systematic review. BMJ. 2002;325:314-36.
- Nelson H, Nygren P, McInerny Y, et al., Screening women and elderly adults for family and intimate partner violence: a review of the evidence for the US Preventive Services Taskforce. Ann Intern Med. 2004;140(5):387-96.
- Feder G, Ramsay J, Dunne D, et al, How far does screening women for domestic (partner) violence in different health-care settings meet criteria for a screening programme? Systematic reviews of nine UK National Screening Committee criteria. Health Technol Assess. 2009;13(16):iii-iv, xi-xiii, 1-113, 137-34.
- Taft A, O’Doherty L, Hegarty K, et al. Screening women for intimate partner violence in healthcare settings. Cochrane Database Syst Rev. 2013;(4):CD007007.
- World Health Organization. Responding to Intimate Partner Violence and Sexual Violence Against Women: WHO Clinical and Policy Guidelines. 2013. World Health Organization, Geneva.
- Garcia-Moreno C, Hegarty K, Lucas d’Oliveira AF, et al. The health-systems response to violence against women. Lancet. 2014;385(9977):1567-79.





Leave a Reply