
Figure 1. Preoperative MRI showing septate uterus with a smooth uterine fundus.
A 67-year-old woman was referred to the gynaecological oncology service with a history of postmenopausal bleeding (PMB) and thickened endometrium on pelvic ultrasonography. The referring gynaecologist was unable to perform endometrial sampling. A review of magnetic resonance imaging (MRI) of the pelvis revealed a septate uterus with thickened endometrium (Figure 1). Clinical examination revealed a narrow-calibre vagina, but no other abnormalities were identified. In view of PMB and abnormal endometrium with a failure to obtain endometrial sample, definitive management in the form of total laparoscopic hysterectomy and bilateral salpingo-oophorectomy was offered, which the patient accepted.
In the operating theatre after surgical preparation and draping, a vaginal fold was noted. On probing, a second very-small-calibre vagina on the left side was noted, separated from the main vagina on the right by a thick septum that ended 1cm short of the introitus. On examination with a paediatric speculum, a smaller cervix was noted on the patient’s left side in addition to the more prominent cervix on the right side. In view of these findings, a laparoscopic hysterectomy was deemed unsafe, since the septum and a duplicated cervix would preclude placement of the colpotomy cup in the fornices needed to allow safe division of the uterine arteries and the vault.
A decision was made to proceed with hysterectomy and bilateral salpingo-oophorectomy via a midline laparotomy in modified Lloyd-Davies position, which allowed easy access for vaginal instrumentation during the procedure, should that become necessary. We had not previously obtained dedicated imaging of the renal tract to rule out urinary tract abnormalities that may be associated with congenital Müllerian duct anomalies (MDAs).
During surgery, the pelvic side wall (PSW) was dissected and both ureters were identified in the PSW and traced down from the pelvic brim to the ureteric tunnel. Due to distorted anatomy at the vaginal angles, the decision was made to open the vagina anteriorly to allow division of the superior end of the septum as well as securing the vaginal angles under vision on either side to avoid ureteric injury. To facilitate this, we used two Hasson ‘S’ shaped retractors that are usually used for open laparoscopy. The narrow retractors could be introduced simultaneously from either side of the septum and allowed the vagina to be opened anteriorly to identify the thick vascular septum in the middle (Figure 2). The septum was divided above a clamp and the edge sutured for haemostasis. The vault angles were secured on either side. The hysterectomy was completed and the vault was closed with interrupted absorbable sutures incorporating the edge of the septum. The decision was made not to divide the septum at this surgery due to its size and because the patient had not been counselled about the additional procedure.
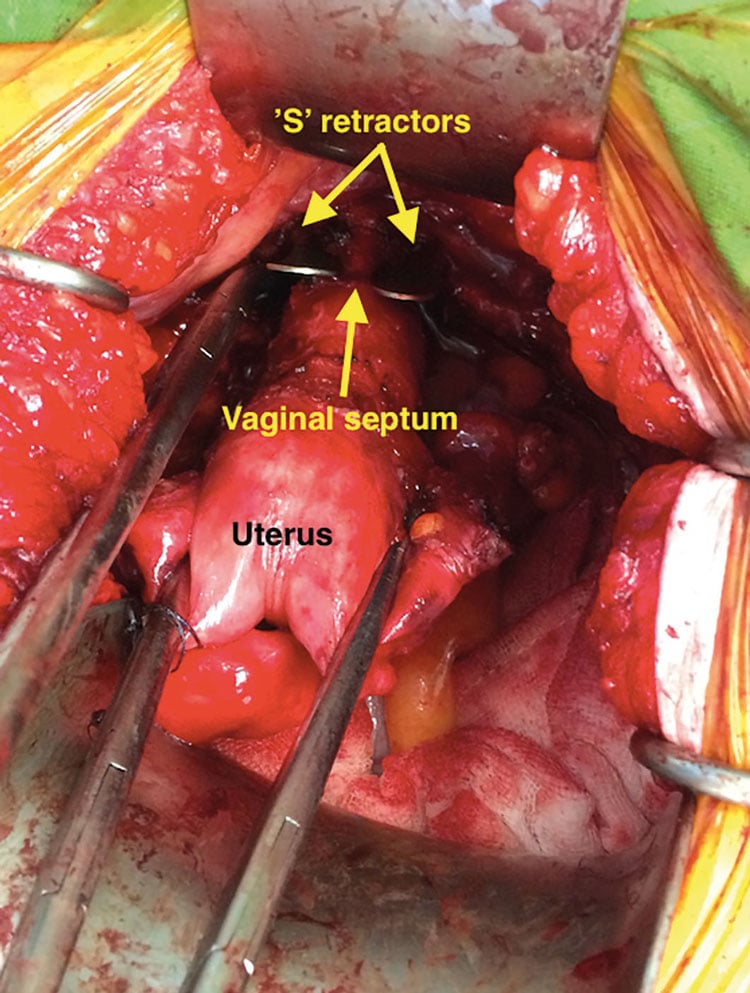
Figure 2. Hysterectomy technique using two ‘S’ retractors to outline the vagina on either side of the septum.
The patient made an uneventful recovery and was informed of the intra-operative findings. Intravenous pyelogram was requested prior to discharge from the hospital and was normal. On final histology, the body of the uterus showed two endometrial cavities separated by a thin, complete septum. There were, however, two distinct cervices with patent endocervical canals. Subsequently, the patient elected to undergo division of the septum. The procedure was carried out eight weeks from the first surgery as a day case and she made an uneventful recovery from the same.
Discussion
This case reflects on the surgical challenge raised by an unusual spectrum of MDAs presenting as a combination of septate uterus, double cervix and vaginal septum that falls outside the existing classification system.1 Cervical duplication is usually associated with uterus didelphys. This triad was first described in 1994, and more recently has been described in just over 20 cases in the English literature by several authors.2 3 4 This case was also unique in that the patient was diagnosed in the seventh decade when she sought medical opinion for postmenopausal bleeding; all previous case reports were of women in the reproductive age group.
This anomaly calls into question the classic theory of unidirectional caudal to cranial Müllerian duct fusion.5 In their proposed classification, Buttram and Gibbons do note that a vaginal septum may be present with didelphys, bicornuate or septate uterus, but felt that the inclusion of vaginal septum in the proposed classification would only complicate matters.6 In 1967, Muller proposed an alternative hypothesis stating that the fusion of the Müllerian ducts may start in the region of uterine isthmus and then proceed in both cranial and caudal directions.7 This theory may explain the more recent observations of the unusual spectrum of congenital anomalies of Müllerian duct development.
Complex developmental anomalies of the Müllerian ducts that do not fit the existing classification system are being increasingly recognised, as is evident from the attempts to reclassify and standardise the nomenclature of these abnormalities by the CONUTA working group.8 The proposed classification allows for recording abnormalities and makes provisions for variations in each anatomical structure of the female genital tract.
With reported diagnostic accuracy of up to 100 per cent, MRI is currently the modality of choice for characterising and evaluating MDAs.9 The clinical correlation between the MRI and surgical findings are reported to be as high as 90 per cent.10 However, the reported high accuracy of MRI has also been challenged. Economy et al reported in 2002 that MRI had a sensitivity of 53 per cent for accurately detecting uterine anomalies confirmed on laparoscopy.11 A radiologist specialising in gynaecological imaging reviewed the patient’s MRI images as a part of surgical planning. While the MRI identified the uterine abnormality, it failed to identify the complex spectrum of developmental anomaly of the urogenital tract.
Renal and urinary tract abnormalities are a significant concern in women with developmental anomalies of the Müllerian duct, with the most common abnormality being unilateral renal agenesis, occurring in about 30 per cent of patients.12 Abnormalities of the renal tract, such as ectopic insertion of ureters, tend to be associated with renal agenesis. The data from the above series would suggest that most renal abnormalities are associated with agenesis, uterus didelphys or unicornuate uterus. Dedicated imaging of the renal tract was not performed prior to the surgery since the severity of MDA was not suspected. Accurate knowledge of the ureteric course is essential for surgeons embarking on complex laparoscopic, open and vaginal surgery. In this case, bilateral kidneys had been identified, there was a clinical need for urgent management as malignancy was suspected, and the surgical team was confident of retroperitoneal dissection and the ability to trace the course of the ureters. Even so, there is a risk of injuring the ureter at the level of its course in the parametrial planes just prior to insertion into the bladder at the time of hysterectomy. Hence, the approach of opening the vagina anteriorly to place a clamp across the vaginal angle in the lateral fornix on either side to obtain a pedicle that was well medial to the course of the ureter. Interestingly, no urological abnormalities were identified in any of the case series or case reports in the literature detailing this unusual anomaly. A postoperative intravenous pyelogram study did not reveal any urological abnormality in our patient.
Conclusion
Current accepted embryological theories do not explain this case of cervical duplication, septate uterus and longitudinal vaginal septum. The current evidence also challenges the accuracy of MRI in definitive diagnosis of MDAs. The use of the proposed ESHRE/ESGE classification system by both clinicians and radiologists may increase the awareness of unusual patterns of MDAs. Knowledge of the patient’s anatomy, especially the urogenital anatomy, is essential for surgeons to safely perform complex gynaecological surgery.
References
- The American Fertility Society. The American Fertility Society classifications of adnexal adhesions, distal tubal occlusion, tubal occlusion secondary to tubal ligation, tubal pregnancies, müllerian anomalies and intrauterine adhesions. Fertil Steril. 1988;49(6):944-55.
- McBean JH, Brumsted JR. Septate uterus with cervical duplication: a rare malformation. Fertil Steril. 1994;62(2):415-7.
- Pavone ME, King JA, Vlahos N. Septate uterus with cervical duplication and a longitudinal vaginal septum: a Müllerian anomaly without a classification. Fertil Steril. 2006;85(2):494.e9-e10.
- Saygili-Yilmaz ES, Erman-Akar M, Bayar D, et al. Septate uterus with a double cervix and longitudinal vaginal septum. J Reprod Med. 2004;49(10):833-6.
- Crosby WM, Hill EC. Embryology of the Müllerian duct system review of present-day theory. Obstet Gynecol. 1962; 20(4):507-15.
- Buttram VC, Gibbons WE. Müllerian anomalies: a proposed classification (an analysis of 144 cases). Fertil Steril. 1979;32(1):40-6.
- Pavone ME, King JA, Vlahos N. Septate uterus with cervical duplication and a longitudinal vaginal septum: a Müllerian anomaly without a classification. Fertil Steril. 2006;85(2):494.e9-e10.
- Gimbizis GF, Gordts S, De Spiezio Sardo A, et al. The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum Reprod. 2013;28(8):2032-44.
- Troiano RN, McCarthy SM. Müllerian duct anomalies: imaging and clinical issues. Radiology. 2004;233:19-34.
- Santos XM, Krishnamurthy R, Bercaw-Pratt JL, Dietrich JE. The utility of ultrasound and magnetic resonance imaging versus surgery for the characterization of müllerian anomalies in the pediatric and adolescent population. J Pediatr Adolesc Gynecol. 2012;25:181-4.
- Economy KE, Barnewolt C, Laufer MR. A comparison of MRI and laparoscopy in detecting pelvic structures in cases of vaginal agenesis. J Pediatr Adolesc Gynecol. 2002;15(2):101-4.
- Hall-Craggs MA, Kirkham A, Creighton SM. Renal and urological abnormalities occurring with Müllerian anomalies. J Pediatr Urol. 2013;9(1):27-32.





Leave a Reply