Over the past decade, traditional methods for acquiring surgical acumen have been challenged at multiple levels. Environmental changes involving fewer ‘hands on’ training hours and increased trainees within the workforce, combined with the development of novel nonsurgical therapies, have all seen our exposure to surgery throughout the training years, and beyond, decrease.
The historic cornerstone of surgical training, ‘see one, do one, teach one’, is no longer an appropriate model in an environment where ‘hands on’ time is at a premium. Furthermore, it is well established that laparoscopy is associated with a prolonged learning curve where the technical skills required are fundamentally different from open surgery. With minimal-access techniques now becoming the gold standard in many major gynaecological procedures, surgical simulation opportunities are fast becoming a training necessity.
Simulation is defined as ‘an educational technique to replace or amplify real experiences with guided experiences, often immersive in nature, that evoke or replicate substantial aspects of the real world in a fully interactive manner’.1 It allows a safe and standardised method of surgical training in a calm, well-controlled environment where the patient is no longer the training commodity. One can acquire and consolidate these basic fine motor skills prior to that first step into the operating theatre.
Simulation recognises and addresses that errors are an integral part of human behaviour, performance and development, and indeed surgical learning curves are a very real and sometimes dangerous thing. It goes some way to try and facilitate that initial surgical training experience without unduly exposing patients to the underlying inherent risk.
With the explosion of simulation training across the world, research into its value and validity continues to be produced. A Cochrane review published in 2013 by Nagendran et al2 summarised the evidence from eight trials looking at the benefits of surgical simulation training in a group of trainees with limited laparoscopic experience. The results showed that when compared to no supplementary training, virtual reality training conferred a higher level of technical accuracy, a reduction in errors, a reduction in the time taken to perform a task, and overall a higher composite operative performance score.
Aggarwal et al3 undertook a study looking at the learning curve for laparoscopic salpingectomy for the management of ectopic pregnancy using virtual reality simulators. They split participants based on prior laparoscopic experience at entry into novice (<10 laparoscopies), intermediate (20–50 laparoscopies) and advanced (>100 laparoscopies), and had them complete a series of ectopic pregnancy simulations over 10 sessions. They showed that while the novice and intermediate group had a steeper and longer learning curve in regards to performance status and time taken to complete the procedure, by the end of the tenth training session, the groups all reached a similar level.
Larsen et al4 took a group of novice (year 1 and 2) trainees and assessed their ability using a validated performance scale to perform a laparoscopic right salpingectomy in the setting of risk-reduction surgery for BRCA carriers. Half of the group were put through a specific surgical simulation training program with basic skills and procedure-specific tasks. They were only able to perform actual surgery once set proficiency criteria were attained during simulation, with the average time spent on the simulator being seven hours and 15 minutes. When comparing the performance status of the two groups, those who had undergone prior simulation training achieved a performance rating equivalent to that of an intermediate level laparoscopist (defined as experience of 20–50 previous procedures), whereas, unsurprisingly, those with no simulation training achieved performance ratings equivalent to that of a novice laparoscopist (defined as experience of fewer than five prior procedures). They were also able to perform the procedure in half the time (12 versus 24 minutes). This clearly shows that via the use of simulator training, one could effectively bypass the early part of the laparoscopic learning curve.
With the evidence supporting the importance of virtual reality training as a surgical training tool, the next subject of debate is the educational package with which it is delivered. Not dissimilar to other forms of teaching, although laparoscopic simulators can be used independently, the mere availability of a trainer does not necessarily correspond to a surgical training benefit.

Simulated laparoscopy has been shown to effectively bypass the early part of the learning curve.
Wilson et al5 recently published on the availability and use of simulation training n New Zealand and Australia. Similarly to data published from surveys of surgical residents overseas, while access to some form of simulation trainer was high (87 per cent), lack of allocated time, lack of supervision, and lack of a formal simulation curriculum were identified as the major barriers to achieving maximal simulation training benefits.
Haerizadeh et al6 coined the concept of the essential “5 W’s” of simulation training curricula to help guide institutions in setting up simulation training services to avoid the all-too-common scenario of available but underused training facilities (Table 1).
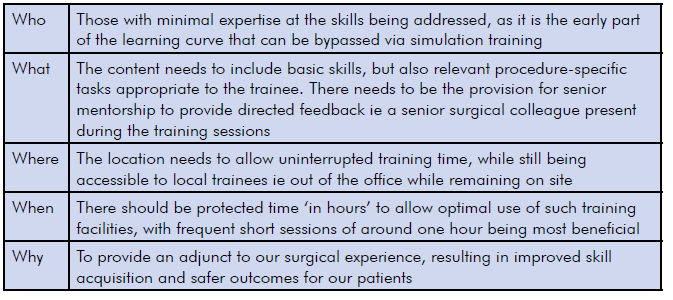
Table 1. The 5 Ws.7
So with all this knowledge to hand, where do we sit with simulation training in New Zealand? Unfortunately, there remains somewhat a postcode lottery with regards to access, support and facilities when it comes to surgical simulation training opportunity. The question remains; with such a wealth of data and evidence that a formal curriculum is necessary, should such training be mandatory? Shetty et al8 found that integration of simulation-based training in a self-directed fashion remained underused and unsuccessful and that mandatory participation was necessary. A recent survey of New Zealand and Australian trainees found that more than 80 per cent believed simulation was beneficial and should be formally added to the RANZCOG curriculum.9
Counties Manukau District Health Board set up a simulation training room in 2011. Funding from the Lion Foundation saw the purchase of two Laparoscopic Simulators (LapSim) and three box trainers. Located in an onsite clinical education centre separate to the clinical department, all new gynaecology trainees are rostered to protected simulation training sessions throughout their placement. The allowance for senior mentorship is included with the presence of a senior surgical educator in the training unit for one half-day session per fortnight. An online anonymous survey of trainees performed after the first year of implementation confirmed that the laparoscopic training program had been well received. Respondents reported an improvement in hand-eye coordination and depth perception, described the training as fun and engrossing, and felt their simulation experience translated to increased confidence in theatre.10
Following such local success, and identification that regional variation in opportunity exists, Counties Manukau and RANZCOG New Zealand teamed up to address this problem with the initiation of a basic laparoscopy course for New Zealand RANZCOG trainees. The concept being all year 1 and 2 registrars attend the course as a mandatory requirement, to ensure a minimum exposure to simulation training. The course is run over three days and includes a variety of simulation training tools, with candidates rotated through 40-minute sessions, with a total exposure of approximately six hours on the LapSim, two hours on box trainers, two hours on models, and six hours in a live animal lab. Course numbers include only four trainees, with two mentors, to allow intensive senior feedback with a two to one ratio. Four courses are run per year to cater for 16 trainees annually nationwide.
Now running for three years, approximately 40 trainees have been through. Course feedback evaluation was available for 55 per cent of participants. Responses were unanimously positive, with 100 per cent rating the course overall as five out of five. Furthermore, when comparing the different types of simulation used throughout, all modalities were deemed beneficial, with average scores between 4.3–4.9 out of five.

Simulated scenarios can come in many different forms. Here teams compete at SimWars, held at the RANZCOG 2016 ASM, as a learning activity.
Clearly, the establishment of this course goes some way to addressing the void in surgical simulation training for our New Zealand trainees. However, with simulation potentially becoming the new cornerstone of early surgical training, continued effort and commitment needs to be made. Formal frameworks need to be developed and delivered in a fashion to allow equal access and opportunity across New Zealand and Australia. Key questions remain unanswered: should simulation training become mandatory or remain a beneficial adjunct where available? Should simulation proficiency assessments in specific surgical tasks be a requirement before being allowed to be the primary operator in real-time theatre? Who is responsible for the development, implementation, monitoring and assessment of simulation training modalities? Who is responsible for the funding required to establish up good-quality facilities?
Moving forward, and we must move forward, these questions need to be answered. We need committed leaders, motivated teachers, receptive trainees, and the underlying drive and buy-in from our key stakeholders, RANZCOG and AGES, who are the governing bodies responsible for O&G specialist and advanced laparoscopic training in Australasia.
References
- Agha RA, Fowler AJ. The role and validity of surgical simulation. International Surgery. 2015;100(2):350-357.
- Nagendran M, Gurusamy KS, Aggarwal R, et al. Virtual reality training for surgical trainees in laparoscopy surgery (Review). Cochrane Database of Systematic Reviews. 2013;8:CD006575.
- Aggarwal R, Tully A, Grantcharov T, et al. Virtual reality simulation training can improve technical skills during laparoscopic salpingectomy for ectopic pregnancy. BJOG. 2006;113:1382-1387.
- Larsen CR, Soerensen JL, Grantcharov TP, et al. Effect of virtual reality training on laparoscopic surgery: randomized controlled trial. BMJ. 2009;338:b1802.
- Wilson E, Janssens S, Hewett DG, et al. Simulation training in obstetrics and gynaecology: what’s happening on the frontline? ANZJOG. 2016;56(5):496-502.
- Haerizadeh J, Frappell J. The role of simulation in surgical skills training in gynaecological endoscopy. Best Practice and Research Clinical Obstetrics and Gynaecology. 2013;27(3):339-347.
- Haerizadeh J, Frappell J. The role of simulation in surgical skills training in gynaecological endoscopy. Best Practice and Research Clinical Obstetrics and Gynaecology. 2013;27(3):339-347.
- Shetty S, Zevin B, Grantcharov TP et al. Perceptions, training experiences, and preferences of surgical residents toward laparoscopic simulation training: a resident survey. Journal of Surgical Education. 2014;71(5):727-733.
- Wilson E, Janssens S, Hewett DG, et al. Simulation training in obstetrics and gynaecology: what’s happening on the frontline? ANZJOG. 2016;56(5):496-502.
- Burgess W, Barclay D. Gynaecology trainees experience of laparoscopic simulation (Lapsim) at Middlemore Hospital: Anonymous internet based survey. RANZCOG ASM Wellington Poster Presentation. 2012.






Leave a Reply