It was not long ago, and certainly prior to the use of ultrasound in pregnancy, that the diagnosis of morbidly adherent placenta was a clinical finding at the time of delivery of the placenta. Adherence of the placenta to the uterine wall carries significant risk of mortality and morbidity to the mother, with emergency caesarean hysterectomy and massive transfusion often being required. The development of high-resolution and Doppler ultrasound as well as adjunctive magnetic resonance imaging (MRI) in pregnancy, has made it possible to diagnose these conditions in up to a half of cases1 2 prior to delivery, and plan for the potential life-threatening complications that it poses.
A number of studies show blood loss and transfusion are significantly lower in women with antenatal diagnosis of abnormally adherent placenta,3 4, mostly because these women are more likely to have preventative therapies for haemorrhage. Several other studies report that planned peripartum hysterectomy also results in less red cell and platelet transfusions,5 as well as less overall blood loss, lower overall complication rates and fewer intensive care unit (ICU) admissions.6
The incidence of placenta accreta has significantly increased, owing to the increasing number of caesareans sections (CS) over time. The Australian average is currently reported as 32.4 per cent7, and the consequences of repeated CS are well documented. In 2006, Silver et al famously reported chances of accreta to be 2.4 times higher after three CS and 8.8 times higher after four CS, compared with one.8 In 2012, the fertility rate in Australia was 1.93 children per woman. This may be thought to offset the rates of accreta mentioned above; however, the condition is still more likely after one CS when compared to a first vaginal delivery and we should suspect it in women with a previous CS, or other uterine surgery, particularly if they have a placenta praevia or increased maternal age.9 10 11
Routine ultrasound at 20 weeks can identify a low-lying placenta or major grade placenta praevia and these women should be followed up with an ultrasound at 32 weeks for placental localisation. Detailed ultrasound interrogation should certainly be performed in the setting of an anterior low placenta in a woman with previous uterine surgery or CS, as the ultrasound findings provide 100 per cent sensitivity. Because the specificity of ultrasound is lower (around 40%), diagnosis and surgical planning can be aided with the additional use of MRI. However, evidence does not support the use of MRI as superior to ultrasound at this stage.12 13 14
Once abnormally adherent placenta is suspected or confirmed, detailed consideration needs to be given to the delivery, including a planned hysterectomy at the time, as best evidence suggests outcomes are improved in this way. This option may not be acceptable to women requiring future fertility and for those women, leaving the placenta in place is an option. This requires discerning postoperative management, as up to 80 per cent (in some series) experience secondary hysterectomy and/or other morbidity.15 16 17
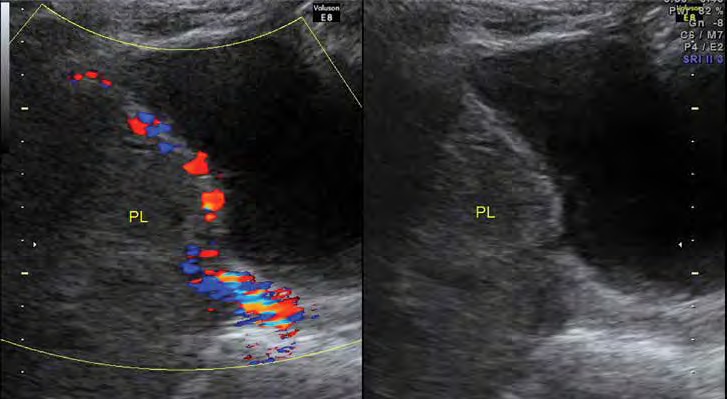
Figure 1. Placenta percreta suspected on ultrasound.
On a day-to-day level, the general obstetrician may consider how they would approach such cases in their own environment, especially if their hospital does not contain a Level 3 adult intensive care unit (ICU) or access to a multidisciplinary team. In the situation where an abnormally adherent placenta is confirmed or is highly suspicious antenatally, a referral to a suitable centre is recommended. When diagnosis of adherent placenta occurs at delivery, which may occur for up to half of placenta accretas diagnosed, the ‘care bundle’ developed by the Royal College of Obstetricians and Gynaecologists,18 is useful. Developed as a response to the findings of the confidential enquiry into maternal deaths,19 the guideline was designed to improve the outcomes associated with placenta praevia/accreta. The approach has been shown to be achievable and practical in a pilot study and suggests the following six practice points be applied in all cases where there is a placenta praevia and a previous CS, or an anterior placenta over-lying the old caesarean scar:
- Consultant obstetrician planned and directly supervising delivery
- Consultant anaesthetist planned and directly supervising anaesthetic at delivery
- Blood and blood products available
- Multidisciplinary involvement in pre-operative planning
- Discussion and consent, including possible interventions (such as hysterectomy, leaving the placenta in place, cell salvage and interventional radiology)Local availability of a Level 2 critical care (ICU) bed.
- Local availability of a Level 2 critical care (ICU) bed.
Further suggestions from the guideline are that women declining blood products be transferred to a centre where cell salvage and interventional radiology are available. Confirming availability of a Level 2 ICU before commencement of the procedure is also recommended.
In a centre with access to Level 3 ICU and a multidisciplinary team, a more integrated approach can be taken and will lead to improved outcomes.20 The team will include obstetricians, gynaecologists or gynae-oncologists, anaesthetists, midwives, neonatologists and possibly all, or some, of the following: haematologists, urologists, interventional radiologists and vascular surgeons. It is important to organise appropriate access to theatre with adequate time allocation for the case. Postoperative recovery in a high dependency unit (HDU) or ICU should be booked and available. Blood products should be matched and available (including consideration of alternatives in the setting of patients who refuse blood products) and cell salvage should be available where possible.
Presurgical planning is best to include:
- Anaesthetic review, in particular the anaesthetic type
- Spinal, combined spinal epidural (CSE) or general anaesthetic (GA).
- Patient consent with clear documentation of risks
- Pain of recovery
- Wound infection
- Bleeding and haemorrhage
- Transfusion of blood and blood products
- Sheehan’s Syndrome
- Trauma to bladder, ureters, bowel or baby
- Deep vein thrombosis and pulmonary embolus
- Prolonged hospitalisation
- Anaemia
- Delayed lactation
- Optimisation of maternal haemoglobin and iron stores
- Intramuscular betamethasone for fetal lung maturation
- Surgical plan for the delivery and hysterectomy
- Skin incision; lower versus midline depending on location of placenta
- Uterine incision; vertical uterine incision (classical) or high transverse uterine incision to avoid entry into placenta. Relevant imaging and a portable ultrasound machine in theatre may be useful for this
- Total or sub-total hysterectomy
- Postoperative venous thromboembolism thromboprophylaxis
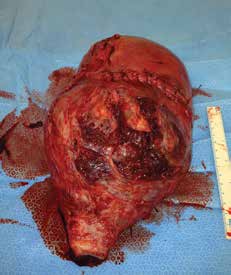
Figure 2. Hysterectomy for percreta
Morbidly adherent placenta will continue to be a significant risk for all women with a previous caesarean section, especially in the presence of placenta praevia and for those of increased maternal age. It carries a significant risk of morbidity and mortality to the mother and is ideally managed in a tertiary centre with access to a multidisciplinary team and Level 3 ICU. There are, however, significant elements of planning that can be performed by obstetricians and gynaecologists in other settings, to minimise poor outcomes.

Figure 3. Patient information videos, available on the College website, can help with the patient consent process.
References
- Bailit JL, Grobman W, Murguia Rice M, et al. Morbidly Adherent Placenta Treatments and Outcomes. Obstet Gynecol.2015;125(3):683-689.
- Fitzpatrick KE, Sellers S, Spark P, et al. The management and outcomes of placenta accreta, increta, and percreta in the UK: a population-based descriptive study. BJOG. 2014;121:62-71.
- Fitzpatrick KE, Sellers S, Spark P, et al. The management and outcomes of placenta accreta, increta, and percreta in the UK: a population-based descriptive study. BJOG. 2014;121:62-71.
- Comstock CH. Antenatal diagnosis of placenta accreta: a review. Ultrasound Obstet Gynecol. 2005;26:98-96.
- Cheng HC, Pelecanos A, Sekar R. Review of peripartum hysterectomy rates at a tertiary Australian hospital. ANZJOG. 2016;56. doi: 10.1111/ajo.12519.
- Briery CM, Rose CH, Hudson WT, et al. Planned vs emergent cesarean hysterectomy. Am J Obstet Gynecol. 2007;197(154):e1-154.e5.
- Hilder L, Zhichao Z, Parker M, et al. Australia’s mothers and babies 2012, in Perinatal statistics series no. 30. Cat. no. PER 69, Australian Institute of Health and Welfare, Editor 2014: Canberra.
- Silver RM, Landon MB, Rouse DJ, et al. Maternal morbidity associated with multiple repeat caesarean deliveries. Obstet Gynecol. 2006;107:1226-1232.
- Fitzpatrick KE, Sellers S, Spark P, et al. The management and outcomes of placenta accreta, increta, and percreta in the UK: a population-based descriptive study. BJOG. 2014;121:62-71.
- Cheng HC, Pelecanos A, Sekar R. Review of peripartum hysterectomy rates at a tertiary Australian hospital. ANZJOG. 2016;56. doi: 10.1111/ajo.12519.
- Fitzpatrick KE, Sellers S, Spark P, et al. Incidence and Risk Factors for Placenta Accreta/Increta/Percreta in the UK:A National Case-Control Study. PLoS ONE. 2012;7(12):e52893. doi:10.1371/journal. pone.0052893.
- Comstock CH. Antenatal diagnosis of placenta accreta: a review. Ultrasound Obstet Gynecol. 2005;26:98-96.
- Riteau A-S, Tassin M, Chambon G, et al. Accuracy of Ultrasonography and Magnetic Resonance Imaging in the Diagnosis of Placenta Accreta. PLoS ONE. 2014;9(4):e94866.doi:10.1371/journal. pone.0094866.
- Berkley EM, Abuhamad AZ. Prenatal Diagnosis of Placenta Accreta. Is Sonography All We Need? J Ultrasound Med. 2013;32:1345-1350.
- Fitzpatrick KE, Sellers S, Spark P, et al. The management and outcomes of placenta accreta, increta, and percreta in the UK: a population-based descriptive study. BJOG. 2014;121:62-71.
- Pather S, Strockyj S, Richards A, et al. Maternal outcome after conservative management of placenta percreta at caesarean section: A report of three cases and a review of the literature. ANZJOG. 2014;54:84-87.
- Steins Bisschop CN, Schaap TP, Vogelvang TE, et al. Invasive placentation and uterus preserving treatment modalities: a systematic review. Arch Gynecol Obstet. 2011;284:491-502
- RCOG Green-top Guideline No. 27. Placenta praevia, placenta praevia accreta and vasa praevia: diagnosis and management. 2011.
- Confidential Enquiry into Maternal and Child Health. Saving Mothers’ Lives: Reviewing maternal deaths to make motherhood safer – 2003–2005.The Seventh Report of the Confidential Enquiries into Maternal Deaths in the UK. London: CEMACH; 2007.
- Russo M, Krenz EI, Hart SR, et al. Multidisciplinary Approach to the Management of Placenta Accreta. The Ochsner Journal. 2011;11:84-88.






Leave a Reply