Louis Washansky was a 55-year-old Cape Town grocer, who in December 1967, received the world’s first transplanted heart. He survived 18 days before succumbing to pneumonia secondary to immunosuppressive drugs. His surgeon, Christiaan Barnard, became a household name and Barnard’s desire to be the first to perform a potentially life-saving operation is easy to understand. But what of Louis Washansky’s motivation to become the first patient? He cannot have been in any doubt that his risk of not waking up was great. By Barnard’s later account, Washansky felt that he had nothing to lose, ‘for a dying man it is not a difficult decision because he knows he is at the end. If a lion chases you to the bank of a river filled with crocodiles, you will leap into the water, convinced you have a chance to swim to the other side. But you would not accept such odds if there were no lion.’1
While there are notable historical exceptions, the progress of medical treatment relies on patients who are willing to be the first to take the step and participate in trials of new treatments. To a great extent, the expectation that new treatments are developed within an ethical framework is somewhat of a recent development and one that is continually under review. While the history of medicine is filled with tales of maverick individuals making momentous discoveries, the flipside is the isolated practitioner drifting ever further from the mainstream. On the one hand, there is Ignaz Semmelweiss and antisepsis; on the other, there is Chelmsford Private Hospital and deep sleep therapy. Consequently, the conduct of research into novel treatments, including consent for participation in research, is now closely regulated.
For many doctors, our experience with consent involves patients receiving treatments that are tried and tested. While there are risks and benefits to these treatments, we are familiar with them. In many cases we can provide written information outlining them to our patients, with RANZCOG providing many useful resources for this interaction. We can often provide local or personal audit data further informing the patient of their potential outcomes, and patients have the ability to seek out independent data sources if they desire. In most cases, we can be confident that our patients have the ability to obtain a reasonable understanding of the proposed course of treatment before deciding whether to go ahead with it.
In the case of novel or experimental treatments, knowledge of the risks and benefits is necessarily less certain and processes must be in place to ensure participants are as well informed as possible before agreeing to participate in these studies. In Australia and New Zealand, the provision of adequate processes lies with need for ethical approval before a practitioner can embark on innovative treatments. All workers in these countries who wish to provide novel treatments will have access to Human Research Ethics Committees (HRECs) through their hospital, university or other organisation. The National Health and Medical Research Council (NHMRC) in Australia is responsible for accrediting HRECs and lists more than 200 associated with government and private organisations.2
RANZCOG, in its Code of Ethical Practice, specifically prescribes that: ‘Where patients are to be approached to consider participation in research, doctors should: ensure that the research has been properly approved by a human research ethics committee.’3
In the case of drug treatments, there is a well-defined pathway of clinical trial phases that provide context to the risk/benefit balance of a particular study.4 (See Table 1.)
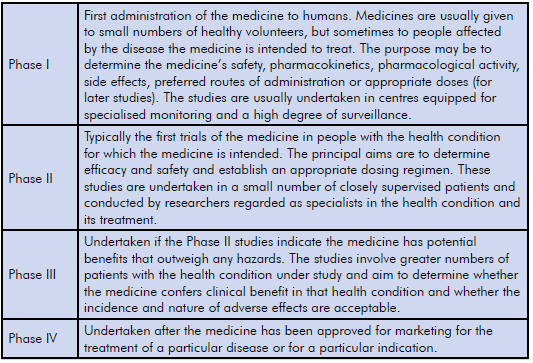
Table 1. Pathway of clinical trial phases.
In the development of drug trials, consent is part of a larger, regulated framework and protocols are agreed upon when the trial is registered. Trials of devices may also follow similar phases, while surgical technique developments may not always be introduced in this way.
While there are common considerations in consenting patients for any clinical procedure, there are particular factors in consent for experimental procedures.
Availability of alternative treatments, including the option to not treat at all
In many cases, our patients are not in the position of Louis Warshansky, the lion has not chased them to the river’s edge and they may have the option of other treatments. Conversely, if the existing treatments were flawless, then we would not be considering alternatives. It is important that patients are made aware of alternatives to the experimental treatment, especially if effective treatments already exist.
Expectation of success
Patients should be provided with evidence supporting the rationale behind a proposed treatment. This evidence could include results from animal research, earlier studies of similar treatments or in the case of surgery, a discussion of the anatomical rationale for the proposed surgery.
Expectation of risks
Experimental treatments vary widely in their possible risks. Compared to established treatments, experimental treatments have a greater potential for unforeseen adverse outcomes, both in the short and long term. While this need not preclude the development of novel treatments, researchers should be careful to inform potential participants of these outcomes, including that they may not necessarily be reversible. A salient case in gynaecology is in the unexpected short- and long-term adverse outcomes suffered by some women receiving pelvic mesh surgery, and whether women were adequately informed of these risks prior to surgery. These cases include some women enrolled in approved clinical trials, and other women receiving the procedures as part of normal clinical care, presumably with consent procedures reflecting both these settings.
Possible conflicts in being both the clinician and researcher
Clinical research spans the range from multi-centre randomised trials where researchers may recruit patients into the trial but are at arm’s length from allocation to treatments and measurement of outcomes, to small local studies where a single clinician may recruit participants, perform the intervention and conduct evaluation. In some cases, a researcher may enrol their own patients in a trial of a new therapeutic technique of their own design. This can lead to a conflict between a desire to help patients by providing them with the latest, hopefully more effective, treatments, and the expectation that patients should have the final choice on whether to proceed with an experimental treatment. On the patient’s part, their decision to consent to a novel treatment may be influenced by a desire to please their treating doctor with whom they may have built up a therapeutic relationship, by agreeing to take part in their trial. This situation risks violating the principle that participation in a trial be truly voluntary. Because of this potential conflict of interest, the NHMRC suggests that ‘where the researcher is also the treating health professional, it should be considered whether an independent person should seek the consent of potential participants.’5
In conclusion, while sharing many of the concepts of consent for any medical procedure or treatment, consent for new or experimental procedures does have additional considerations. Clinicians and researchers need to be aware of these differences and incorporate them in to their practice. In many cases novel procedures should be conducted with the approval of a HREC, with appropriate recruitment and consent forming part of the approval process.
References
- McRae D. Every Second Counts: The Extraordinary Race to Transplant the First Human Heart. 2007. Penguin.
- www.nhmrc.gov.au/_files_nhmrc/file/health_ethics/human/att_2_-_list_of_ human_research_ethics_committees_ registered_with_nhmrc_june_2016.pdf. Accessed 9 July 2016.
- www.ranzcog.edu.au/the-ranzcog/policies-and-guidelines/code-of-ethical-practice. html. Updated June 2012. Accessed 9 July 2016.
- www.nhmrc.gov.au/book/chapter-3-3-interventions-and-therapies-including-clinical-and-non-clinical-trials-and. Accessed 9 July 2016.
- www.nhmrc.gov.au/book/chapter-3-3-interventions-and-therapies-including-clinical-and-non-clinical-trials-and. Accessed 9 July 2016.






Leave a Reply