Thalidomide (alpha-phthalimido-glutarimide) was initially developed as an anticonvulsant drug, but was ultimately found to be unsuitable for this indication. However, during trials it was inadvertently noted to have sedating properties. It was first introduced into clinical medicine in Germany, in 1957, and subsequently was distributed in Europe, the UK and Australia by numerous companies under several different trade names, including Contergan, Distaval and Kevadon. Thalidomide was marketed for a wide range of clinical indications, although its main use was as a sedative/tranquiliser. Later, compound preparations including thalidomide were introduced for a number of indications including asthma (Asmaval), hypertension (Tensival) and migraine (Valgraine). The drug was also prescribed to women to treat morning sickness during early pregnancy.
The first known case of thalidomide embryopathy was in a baby girl born with absent ears in Germany in 1956. Her father worked for the company (Grünenthal) making the pills and gave his wife free samples during early pregnancy. Several other cases related to women taking samples before the drug was marketed in Germany from 1957.1
In 1961, a German paediatrician, Lenz, reported two cases of babies with congenital limb anomalies at a German paediatrics conference and postulated that maternal exposure to thalidomide during pregnancy was the underlying cause of these defects.2 One month later, in December 1961, William McBride, an Australian obstetrician, wrote a letter to the Lancet describing cases of unusual, severe limb defects in babies born to mothers who had taken thalidomide in early pregnancy.3
McBride noted that approximately 20 per cent of exposed infants had evidence of skeletal anomalies including polydactyly, syndactyly and limb reduction defects. Subsequent to these initial cases, further reports of affected babies came from numerous countries worldwide where the drug was available including, among others, the UK, Kenya, Sweden, Japan, Belgium, Switzerland, Canada, Peru and Brazil. There were very few cases reported from the USA, as the FDA had not allowed the drug to be released except for clinical trials, owing to concerns about reports from Europe of irreversible peripheral neuropathy and that a drug that caused nerve damage could potentially have significant effects on embryonic development. Since the drug was available over the counter in Germany, there were more affected children there than anywhere else in the world.
As the rate of thalidomide use increased in the late 1950s and early 1960s, there was a rise in the number of cases of thalidomide embryopathy, with the peaks occurring in 1961 and 1962 in Germany, with 1515 and 927 cases reported, respectively. Because the drug became available in different countries at different times, it was possible to track the epidemic of cases that became apparent seven to eight months after the drug was first introduced on to the market.1 For example,in Canada, thalidomide was not marketed until April 1961 and, consequently, the epidemic of cases did not begin before December 1961.4
Owing to concerns raised about potential teratogenic effects, thalidomide was withdrawn from the market. However, just as with its introduction, withdrawal occurred over a period of time and, consequently, the end of the epidemic of thalidomide embryopathy could be documented according to when the drug was withdrawn from the market in different countries. In Germany, thalidomide was withdrawn in November 1961 and, as expected, there was a sharp decline in the number of cases reported after July/August 1962 (eight to nine months after withdrawal).5
In recent times, thalidomide has emerged as a potential treatment for a number of conditions, including: hepatocellular carcinoma, chronic graft-versus-host disease, rash owing to systemic lupus erythematosus, Behçet’s syndrome, inflammatory bowel disease, prostate cancer, metastatic breast cancer, rheumatoid arthritis and for complications of AIDS (aphthous ulcers, diarrhoea, macular degeneration, cachexia and Kaposi’s sarcoma). In 1998, the FDA approved its use for the treatment of erythema nodosum leprosum (ENL).6
Since then, a number of cases of thalidomide embryopathy have been reported from South America,7 but none from the USA, where a strict program of prescribing and dispensing (STEPs Program) was implemented and has apparently been successful to date in preventing thalidomide-exposed pregnancies.8
Thalidomide is a true teratogen in that it can induce birth defects in the absence of maternal toxicity. One of the most important principles of teratology is that there is a critical period during which time an organism is most susceptible to the teratogenic effects of the particular agent. This critical period differs according to species (where there are different lengths of gestation).
In humans, the critical period of exposure to thalidomide is 34–50 days after the last menstrual period (LMP). In biological and basic scientific texts gestational age is often quoted as post conception, which generally occurs two weeks after the LMP. Thus the critical period for thalidomide exposure is 20–36 days after conception. Because different organ systems develop at different times, the types of birth defects seen following exposure to thalidomide depend on the gestational timing of the exposure. It is also important to emphasise that thalidomide exposure occurring after the critical period of development would thus not be expected to cause structural anomalies.
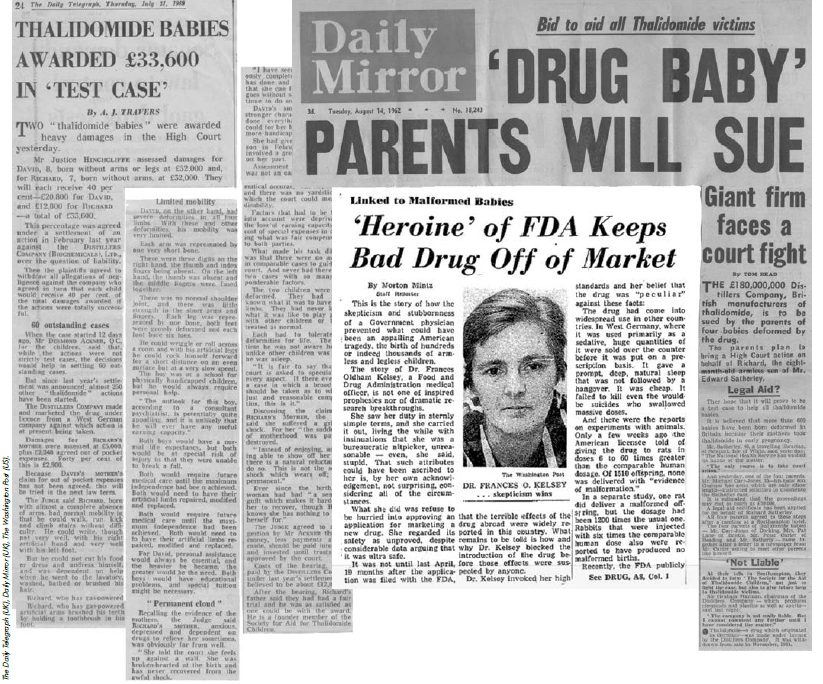
Headlines around the world: the thalidomide tragedy led to tighter control of new medicines, in general, and prescribing for pregnant women, in particular.
Limb defects are probably the most recognisable and well known of thalidomide’s effects, but the drug was able to induce malformations in a large number of human systems including skeletal, cardiovascular, gastro-intestinal, genito-urinary, cranio-facial and central nervous systems. Congenital malformations associated with approximate time periods within this 17-day time period include (days after LMP): anotia (34–38 days), microtia (39–43 days), thumb duplication (35–38 days), thumb aplasia (35–43 days), thumb hypoplasia (38–40 days), eye defects (35– 42 days), cardiovascular defects (36–45 days), vaginal duplication (35–39 days), cranial nerve palsy (35–37 days), amelia of upper limbs (38–43 days), phocomelia of upper limbs (38 to 47–49 days), amelia of lower limbs (41–45 days), phocomelia of lower limbs (40 or 42–47 days), choanal atresia (43–46 days), duodenal atresia (40–47 days), anal atresia (41–43 days), gallbladder aplasia (42–43 days), pyloric stenosis (40–47 days), duodenal stenosis (41–48 days), rectal stenosis (49–50 days), ectopic kidney and hydronephrosis (38–43 days) and abnormal lobation of lungs (43–46 days).9 10
Estimates of the risk of development of congenital malformations in offspringexposed to thalidomide during the critical period range from ten to 50 per cent.11 The reason there is such a large degree of uncertainty in this estimate is due to the lack of epidemiological studies, as well as the inability to determine the number of exposed but unaffected children. It is also worth noting that the early mortality rate among babies exposed to thalidomide was approximately 40 per cent, owing to the presence of severe internal malformations (such as, for example, cardiovascular and gastro-intestinal).
It is still unclear what factors determined whether or not an exposed embryo was affected and, if so, which systems were involved. An interesting case of a twin pregnancy was reported with the offspring showing very different manifestations of thalidomide embryopathy after the same exposure. The first twin was a female weighing 2211g at birth born with duodenal atresia, a recto-perineal fistula and hypoplastic dislocated thumbs. The second twin, a male weighing 2240g at birth, had phocomelia of both upper limbs as well as missing/hypoplastic digits on both hands and a midline hemangioma of the forehead.12
Thalidomide significantly changed the way in which risks of medication in pregnancy were perceived and how medications were assessed in terms of potential reproductive risks. This has had both positive and negative ramifications.
As was recognised at the time, the ramifications of the thalidomide tragedy will last for a generation or more. (Wellcome Library, London, reproduced under licence CC BY 4.0.)
In 1963, as a direct consequence of the thalidomide tragedy, the Commonwealth Department of Health established the Australian Drug Evaluation Committee (ADEC) as an independent committee to advise on the safety of new drugs being introduced into Australia and to monitor and evaluate potential adverse effects of drugs already available. In 2010, ADEC was replaced by the Advisory Committee on Prescription Medicines (ACPM). The Australian categorisation of risk of drug use in pregnancy (A-X) was established by ADEC, is still in use today and largely dictates medication prescribing in pregnancy and how risks of medications in pregnancy are perceived by both healthcare professionals and consumers.
Although ADEC’s aim was to prevent a similar tragedy occurring with any future medications, what has actually occurred is that healthcare professionals have become extremely cautious and risk-averse about prescribing (or dispensing) medications during pregnancy because of perceived (and often greatly exaggerated) fears of teratogenicity, not considering that the risks of untreated illness in most cases are far greater than the often theoretical risks of teratogenicity. This has resulted in large numbers of women being untreated or under-treated for significant medical conditions that could adversely affect their health and that of their unborn baby during pregnancy. In addition, some women go so far as to terminate or seriously consider terminating otherwise-wanted pregnancies because of these fears of teratogenicity.
Fortunately, there has not been another ‘thalidomide’ since the early 1960s and hopefully such a tragedy will not occur in the future. However, it is important that we enter a new era of rational evidence-based prescribing and medication use in pregnancy so that both women and healthcare professionals understand the pros and cons of appropriate medication use during pregnancy and (breastfeeding) and can make rational decisions, thereby optimising the health of pregnant women and their babies.
References
- Lenz W. A short history of thalidomide. Teratology. 1988; 38:203-215.
- Lenz W. Thalidomide and congenital abnormalities. Lancet. 1962; 1:45.
- McBride WG. Thalidomide and congenital abnormalities. Lancet. 1961; 2:1358.
- Webb JT. Canadian thalidomide experiences. Can Med Assoc J. 1963; 89:987-992.
- Lenz W. A short history of thalidomide.Teratology. 1988; 38:203-215.
- Schuler-Faccini L, Soares RCF, de Sousa ACM, et al. New cases of thalidomide embryopathy in Brazil. Birth Defects Research (Part A). 2007; 79:671-672.
- Friedman JM, Kimmel CA. Teratology Society 1988 Public Affairs Committee symposium: The new thalidomide era: dealing with the risks. 1999; 59:120-123.
- Public Affairs Committee, Teratology Society. Teratology Society Public Affairs Committee position paper: Thalidomide. Teratology. 2000;62:172-3.
- Newman CGH. The thalidomide syndrome: risks of exposure and spectrum of malformations. Clin Perinatol. 1986; 13:555-571.
- 13 Nowack E. The sensitive period of thalidomide embryopathy. Humangenetik. 1965; 1:516-536.
- Nowack E. The sensitive period of thalidomide embryopathy. Humangenetik. 1965; 1:516-536.
- Mellin GW, Katzenstein M. The saga of thalidomide. Neuropathy to embryopathy with case reports of congenital anomalies. N Engl J Med. 1962; 267:1184-1193.





Leave a Reply