In 1977, my wife and I attended a small gathering of friends in London, where we were living at the time. Ari, a visiting young American gay man performed bharatanatyam, a South Indian dance. A couple of years later, I heard that Ari was declining rapidly with some sort of baffling immune condition. Then I heard that Ari had died. Later, I remember reading a small article in the Times announcing, on 5 June 1981, the recognition of a new and mysterious immune disease, later called AIDS, now called HIV infection.
In 1981, on my way to an interview for a possible alcohol and drug position at St Vincent’s Hospital, Sydney, a young woman in a dirty grey singlet and sporting impressive track marks approached me in the street to enquire whether I would ‘like to have a good time’. I replied ‘No, thank you’, but I decided that this was the hospital I would love to work at. I got the job.
I will never forget the first case of AIDS admitted under my care at St Vincent’s Hospital in the mid-1980s: a young gay New Zealander who had come to Sydney after several years living in the USA. I spent a lot of time doing oesophagoscopies and sigmoidoscopies on severely ill gay young men to diagnose a condition that was then untreatable and often rapidly terminal.
Bit by bit, the nature of this epidemic became clearer. The magnitude of the threat was uncertain, but it was clear from the outset that potentially this was a serious threat to the health, well-being and economy of Australia. If anything, the early assessments turned out to be far too optimistic. The media largely ignored the epidemic until the Grim Reaper advertisements began appearing in April 1987. Though intended to persuade the (then) Treasurer, Paul Keating, to allocate sufficient funds for AIDS in the next Budget, the advertisements shifted AIDS from small paragraphs buried on an inside page of our newspapers to headlines on the first page. The Treasurer put aside sufficient funds in the 1987 Budget for a vigorous national response to HIV.

In 1987, the National Advisory Committee on AIDS ran a television advertising campaign depicting the
Grim Reaper bowling in a bowling alley and knocking over men, women, and child ‘pins’, representing
AIDS victims. It is still considered a landmark in advertising and shifted the focus of the debate.
St Vincent’s Hospital was in the epicentre of this new epidemic. Thousands of gay men in the neighbourhood had rapidly become infected in the early 1980s. It was clear that there was a frightening risk of a cascade of HIV infections starting among gay men, spreading from gay men who used drugs to their heterosexual counterparts through needle sharing and then spreading to the general community through sexual contact. Once the genie was out of the bottle, getting it back in again was going to be a nightmare. I spent sleepless nights worrying about this.
A group of healthcare workers and people who used drugs started meeting regularly to discuss what we should do. It was clear that starting a program to swap sterile needles and syringes for used injecting equipment was the most urgent priority. I had been asked to coordinate a national workshop on cocaine and allocated Dr Stan Yancovits, an infectious disease physician from New York, to be the main speaker. I rang Dr Yancovits and asked him if he would be willing to speak about HIV while in Australia and to also, perhaps, support starting needle exchange. He was more than willing. He spoke about a nurse in his hospital who had died from AIDS after being infected years earlier by a previous husband, leaving behind her second husband and a number of small children. Dr Yancovits described how she had written out her will while dying. Chilling stuff. I wrote many submissions to the NSW Health Department begging to be allowed to start a needle syringe program. Later, a friend working in the Health Department was asked to clean up some shelves and came across 13 separate submissions written by me. All had been declined or ignored.
We also knew that the methadone program had to be expanded and liberalised. I arranged for Dr Yancovits to speak to the state committee. The committee then agreed to support expansion and liberalisation. The numbers on the NSW methadone program started to rapidly increase.We eventually realised that the NSW Health Department was never going to approve a needle syringe program before the epidemic had started. So we had to resort to civil disobedience. The first needle and syringe was handed out on 13 November 1986. It was a big decision for every member of the group. My regret is that we did not start earlier. Now, almost 20 years later, the prevalence of HIV among Australians who inject drugs (and have no other risk factors) is still less than two per cent. Half the needle syringe programs in the world were started by civil disobedience. Some countries were not as lucky and, with no needle syringe programs and minimal or no methadone program, HIV spread among and from people who inject drugs to the general community. In Thailand, the prevalence of HIV among people who inject drugs increased from less than one per cent to more than 40 per cent in ten months in 1987. Within five years in the north-west of the country, one-in-12 pregnant women and one-in-six male military recruits had HIV infection. That could also have been Australia’s story.
Much as I support research, I was delighted to learn that a study of HIV infection in children run from the Sydney Children’s Hospital in the 1990s had to be cancelled as there were not enough HIV-infected children to carry out the study.
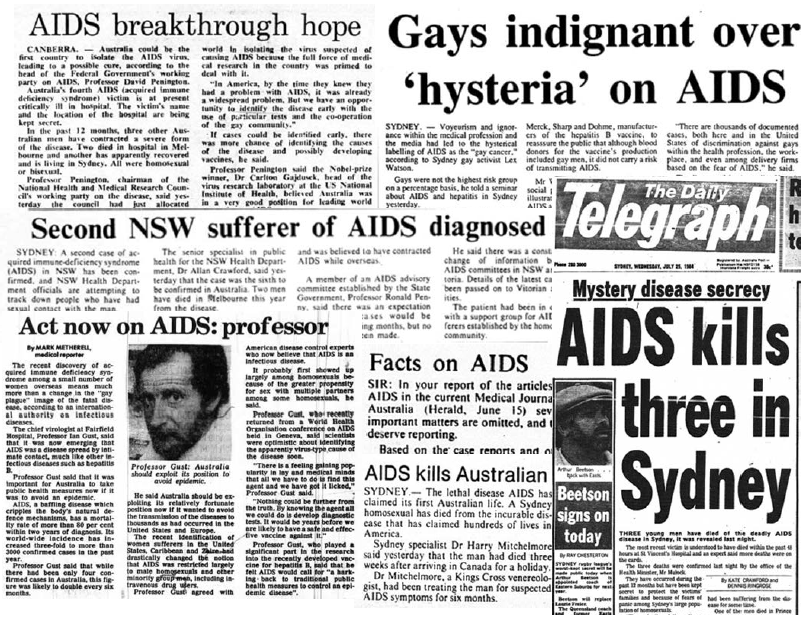
Newspaper stories from Australia in 1983 and 1984, as news of the first cases of AIDS broke. Clippings collected by Paul Kidd (http://realtimeaids.com). Copyright in quoted or reproduced media stories and articles remains with the holder and materials are reproduced for non-commercial, educational purposes only
Although I have received a lot of credit for this response, the truth is that it could never have happened without many others, healthcare workers and people who inject drugs, sharing the work and the risk. We were lucky to have the strong support of many senior health department officials, policymakers and politicians. Peter Baume, the (then) Shadow Health Minister, had to persuade the (then) Opposition Leader, John Howard, and Neal Blewett, the (then) Health Minister, had the easier task of persuading the (then) Prime Minister, Bob Hawke to allow pragmatism to triumph over short-term political gains.
One of the lessons from this episode is if you want to make some serious health gains, the target population has to be meaningfully involved every step of the way.




Leave a Reply