The morphology scan performed at 18–22 weeks has become a routine part of modern obstetric practice. As obstetricians, it is important that we understand what the scan involves and its limitations to respond to this question appropriately.
The Australasian Society of Ultrasound in Medicine (ASUM) has listed the anatomic structures that need to be visualised during the morphology scan (see Table 1), essentially ruling out a list of structural abnormalities. However, each scanning unit will have their own protocol and may have slightly different variations of what is visualised, documented and reported. If any abnormality is suspected or if the operator is unsure, it is recommended that the patient should be referred to a specialist service that can assess and counsel the patient appropriately.
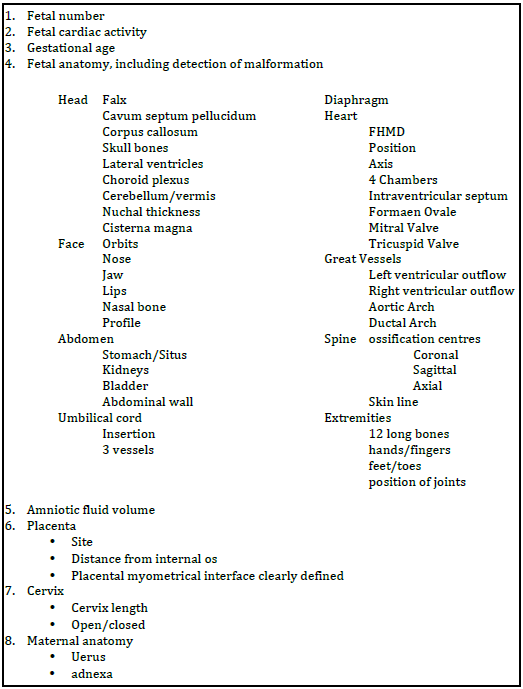
Table 1: ASUM examination checklist 1
ASUM requires that fetal number and viability are confirmed, followed by estimation of gestational age. Estimation of gestational age by biometry at this time is most accurate using the head circumference, with a margin of error +/-7 days.2 3 This ensures growth is appropriate with prior dating, sets a baseline if there are concerns regarding growth later and guides accurate decisions around timing of delivery, for example, postdates induction of labour.4 The position of the placenta and its relation to the internal os is examined. When a low-lying placenta is identified a follow up scan is recommended at 34 weeks, a repeat scan should only be necessary in approximately five per cent of all cases.5 The cervix is assessed on a transabdominal scan and, if concerns are raised, a transvaginal scan is then undertaken. If a short cervix is discovered, treatment options of progesterone or cerclage may be considered.
The detection of structural abnormalities at 18–20 weeks allows parents the option of further invasive testing for chromosomal analysis or genetic testing and the option not to continue with the pregnancy in the case of major abnormalities. For parents that continue with the pregnancy, it allows time for appropriate planning for fetal therapy and ongoing monitoring. In addition, time is available for planning perinatal management with multidisciplinary team input for neonatal or palliative care.
What doesn’t a normal morphology scan rule out?
It is tempting to say ‘everything is normal’ after a morphology scan is performed; however, not all abnormalities can be ruled out. Fetal abnormalities may be structural or functional and the underlying cause may be chromosomal, genetic, infective, teratogenic, vascular, mechanical or unknown. Ultrasound has the ability to detect structural abnormalities. Functional abnormality may be inferred from structural abnormalities, be obvious (for example, fetal akinesia syndromes), or may not be detectable by ultrasound.
The detection of chromosomal or genetic abnormalities at the morphology scan is dependent on the association with structural malformation. When there are multiple abnormalities detected on scan, the possibility of a chromosomal or genetic abnormality is considered and invasive testing with amniocentesis for karyotype or specific gene tests offered. Ultrasound alone cannot rule out a chromosomal or genetic abnormality and studies show a low detection rate even for the common aneuplodies.6 In the majority of cases, Trisomy 13 and 18 fetuses will present with multiple abnormalities, but up to 40 per cent of Trisomy 21 fetuses may not have an abnormality detected.7 For a genetic condition such as cystic fibrosis, the most common autosomal recessive condition in the Caucasian population, features suspicious for this such as echogenic bowel may or may not be evident on ultrasound in an affected fetus.
Why can’t we say ‘it’s normal’ after a normal scan?
In a systematic review based on 11 studies to examine the use of routine second trimester ultrasound to detect fetal anomalies, the overall prevalence of fetal anomaly was 2.09 per cent (range 0.76–2.45 per cent) and detection of fetal anomaly was 44.7 per cent (range of 15–85.3 per cent).8 A Cochrane review of routine ultrasound before the 24th week of pregnancy, found significantly increased detection of fetal abnormalities, RR 3.46 (95 per cent CI 1.67–7.14; two trials, 387 patients).9
Three large, randomised studies have examined the ability of the routine morphology scan to detect fetal abnormalities; the key findings are summarised in Table 2.
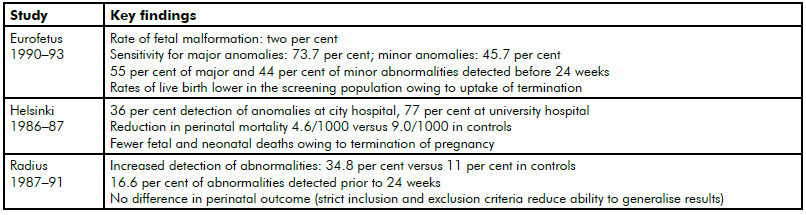
Table 2. A summary of relevant studies’ findings.
The Eurofetus study was the largest and demonstrated the disparity in detection rates for different organ systems, with cardiac anomalies having the lowest rate of detection: the sensitivity for major congenital heart disease was 39 per cent in comparison to central nervous system at 88 per cent and urogenital malformations 89 per cent. The Helsinki and Radius Trials were conducted in the 1980s and we hope, with the increases in ultrasound technology and operator experience, that these detection rates would have improved.
Ultrasound is a user-dependant modality and, as such, better results are expected in more experienced hands and with better equipment. Improved detection is demonstrated in a tertiary setting.10 11 12 Gestation affects the scan as fetal anatomy is better demonstrated at 22–24 weeks than 18–20 weeks. In addition, maternal body habitus plays an important role in the ability of the sonographer to detect abnormalities. Some abnormalities are subtle and may be missed even by an experienced sonographer. There are many other abnormalities that may only become evident in the third trimester, for example, some forms of skeletal dysplasias or a tracheo-oesophageal anomaly.
What if soft markers are seen at the morphology scan?
Many practices will report on soft markers and recommend further investigations. Soft markers are ultrasound findings that may be transient and in themselves have little or no pathological significance, but are thought to be seen more commonly in fetuses with congenital abnormalities, particularity karyotypic abnormalities. They may be seen in 11–17 per cent of normal fetuses.13 The most commonly reported soft markers include choroid plexus cysts (CPC), renal pelvic dilatation and echogenic cardiac foci (ECF). A recent fetal imaging workshop, attended by experts from obstetrics, paediatrics and radiology, recommended no follow up for CPC and ECF in the context of prior low-risk screening or non-invasive prenatal testing (NIPT), while renal pelvic dilatation >4mm should be followed up with a scan at 32 weeks and postnatally, if indicated (to detect renal abnormalities). In those that don’t have a prior risk assessment, NIPT would be a reasonable next assessment option, but is not accessible to all patients owing to its cost.14 Nuchal thickening and absent or hypoplastic nasal bone are the two markers for which genetic counselling regarding the risk of Down syndrome is recommended. Short long bones and echogenic bowel need review not only to consider the possibility of a chromosomal abnormality, but also for specific causes such as skeletal dysplasia in the case of short long bones and infection; cystic fibrosis, growth restriction, intramniotic bleeding and gastrointestinal obstruction in the case of echogenic bowel.
Detection and reporting of soft markers is controversial because this information is anxiety-provoking for patients, requires considerable time for counselling and may lead to invasive prenatal testing with an associated risk of miscarriage; however, parents should be allowed to make an informed decision.
So, what does a normal scan mean?
When counselling our patients, the emphasis should be that there is no abnormality detected within the limits of the examination. The additional variables that need to be considered are maternal body habitus, gestation at assessment, the level of expertise at the imaging practice and so forth. We need to admit no test has been devised so far that rules out all structural and functional abnormalities in the fetus to allow us to say that everything is normal.
References
- ASUM guidelines for the Mid Trimester Obstetric Scan. 2014.
- Hadlock FP, Harrist RB, Martinez-Poyer J. How accurate is second trimester fetal dating? J Ultrasound Med. 1991;10(10):557-561.
- Law RG, MacRae KD. Head circumference as an index of fetal age. J Ultrasound Med. 1982;1(7):281-288.
- Neilson JP. Ultrasound for fetal assessment in early pregnancy. Cochrane Database Syst Rev. 2010;(4):CD000182.
- ASUM guidelines for the Mid Trimester Obstetric Scan. 2014.
- Bricker, L. Garcia J. Ultrasound screening in pregnancy: a systematic review of clinical effectiveness, cost-effectiveness and women’s views. Health Technol Assess (Rockv). 2000;4(16).
- Papp C, Szigeti Z, Tóth-Pál E, Hajdú J, Joó JG, Papp Z. Ultrasonographic findings of fetal aneuploidies in the second trimester – Our experiences. Fetal Diagn Ther. 2008;23:105-113.
- Bricker, L. Garcia J. Ultrasound screening in pregnancy: a systematic review of clinical effectiveness, cost-effectiveness and women’s views. Health Technol Assess (Rockv). 2000;4(16).
- Neilson JP. Ultrasound for fetal assessment in early pregnancy. Cochrane Database Syst Rev. 2010;(4):CD000182.
- Saari-Kemppainen Aul, Karjalainen Olav, Ylostalo P, Heinonen OllP. Ultrasound Screening and Perinatal Mortality: controlled trial os systematic one-stage screening in pregnancy. Lancet. 1990;18:387-391. doi:10.1097/00006254-199107000-00004.
- Ewigman,Bernard. Crane, James. Friggoletto F et al. Effect of Prenatal Ultraound Screening on Perinatal Outcome. N Engl J Med. 1993;329(12):821-828.
- Grandjean H, Larroque D, Levi S. The performance of routine ultrasonographic screening of pregnancies in the Eurofetus Study. Am J Obstet Gynecol. 1999;181:446-454. doi:10.1016/S0002-9378(99)70577-6.
- Breathnach FM, Fleming A, Malone FD. The second trimester genetic sonogram. Am J Med Genet Part C Semin Med Genet. 2007;145(1):62-72.
- Reddy UM, Abuhamad AZ, Levine D, Saade GR. Fetal imaging: executive summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, American Institute of Ultrasound in Medicine, American College of Obstetricians and Gynecology. Obstet Gynecol. 2014;123(5):1070-82.






Leave a Reply