The role of imaging in the diagnostic work up of acute pelvic pain.
The initial diagnostic work up of the non-pregnant gynaecological patient with acute abdominal pain includes the taking of a thorough history, a full clinical examination, laboratory tests and imaging.
Differential diagnoses include cyst accident, dysmenorrhea, mittelschmerz, endometriosis, ovarian torsion, pelvic inflammatory disease and tubo-ovarian abscess, fibroid degeneration or torsion, or a non-gynaecological cause, such as appendicitis, constipation, diverticulitis, mesenteric adenitis or urinary tract infection.
Clinicians often request scans with one or more diagnoses in mind based on clinical findings. The role of imaging is to further delineate this differential, guiding management that may range from conservative to medical to surgical.
Ultrasound is usually the modality of choice as it is generally readily available, inexpensive and does not expose the patient to radiation.1 In some cases, plain x-ray or cross-sectional imaging such as computed tomography (CT) or magnetic resonance imaging (MRI) may also provide further information, or help to delineate ultrasound findings.
Ovarian cyst accident
Cyst accidents refer to the rupture or haemorrhage of physiological cysts. These two conditions are generally benign and self-limiting, and their diagnosis can help to rule out other causes of acute pain and, therefore, avoid unnecessary surgery or further investigation.
Ovarian cysts are common findings on ultrasound scan. Transabdominal (TA) scans can help to characterise large cysts, while transvaginal (TV) probes allow the sonographer to get closer to the ovaries and therefore provide more detail, particularly in regard to delineating a cyst’s relationship to the ovary and/or Fallopian tube.2
Physiological cysts are typically anechoic with thin, smooth walls and posterior acoustic enhancement.3 Cyst rupture may be characterised by the presence of anechoic free pelvic fluid with or without a simple cyst. With haemorrhagic cyst rupture fluid is more complex, appearing echogenic, with mobile debris.
The appearances of haemorrhagic cysts vary depending on their acuity. A fresh haemorrhage will demonstrate low level, uniform echoes that over time organise and demonstrate septations and/or a retracted echogenic clot.4 5
As ultrasound is a dynamic technique, probe tenderness may localise pain to pathology.
Ovarian cysts (particularly large cysts) are commonly seen in cases of ovarian torsion and it is important to attempt to rule this out in the presence of acute pain. This is discussed further below.
Endometrioma
Endometrioma classically appear as lesions with homogenous, low-level internal echoes (see Figure 1). They can be multi-loculated. Hyperechoic wall foci, which appear as small ‘dots’ on ultrasound, are highly specific but not common.6 In practice, endometrioma are difficult to distinguish from haemorrhagic cysts. Bilateral lesions are more likely to be endometrioma. If unsure as to whether the cyst is an endometrioma or an acute haemorrhagic cyst, a follow-up scan in six weeks will usually demonstrate resolution of a haemorrhagic cyst or persistence of an endometrioma.
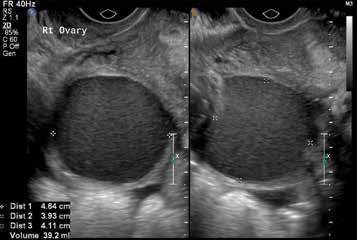
Figure 1. Endometrioma. Transvaginal ultrasound demonstrates a right ovarian lesion with homogeneous low level internal echoes. In this patient, a similar lesion was also present in the contralateral ovary.
If endometriosis is suspected as the cause of acute pelvic pain, ultrasound can be used to assess for endometrioma, but is insensitive for the detection of endometrial implants. Therefore, MRI is the imaging modality of choice for the detection of these endometrial deposits.
Ovarian torsion
Ovarian torsion is a gynaecological emergency that requires prompt surgical treatment. It is notoriously difficult to diagnose, with symptoms and signs varying markedly between patients.7
Ovarian torsion on greyscale ultrasound is associated with enlarged ovaries that may be hyper- or hypoechoic, with enlarged, peripherally displaced follicles, owing to increased interstitial pressure and impaired lymphatic and venous drainage8 (see Figure 2). This increase in pressure also causes the release of transudate, which is seen as anechoic pelvic free fluid. Ovarian torsion is more common in the presence of ovarian cysts, particularly those greater than 5cm in diameter.9
A twisted vascular pedicle is diagnostic when present. This is seen as a round, anechoic structure with multiple concentric echoic stripes.10
Colour-flow Doppler is useful (see Figure 2). Absent arterial and/or venous flow is strongly suggestive of torsion, particularly when associated with some or all of the above findings. Flow may also be seen to be present, but abnormal when compared to the contralateral ovary.11 Cases of intermittent torsion are common and ovarian torsion cannot be ruled out even when normal flow is documented.
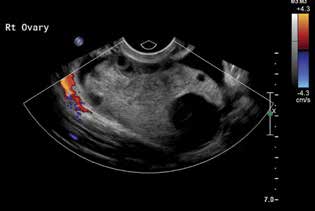
Figure 2. Ovarian torsion. Transvaginal ultrasound image demonstrating an enlarged ovary with peripherally displaced follicles, mild increased central echogenicity and absence of colour flow.
Tubo-ovarian abscess
Pelvic inflammatory disease (PID) is a clinical diagnosis and may be associated with a normal pelvic ultrasound scan.12 PID may be supported by visualisation of hydrosalpinges (fluid filled structures adjacent to the uterus), free fluid or enlarged ovaries.13
Tubo-ovarian abscesses (TOA) are seen on ultrasound as multiloculated complex masses with internal debris, septations, irregular thick walls and increased vascularity. They are often bilateral and tender to probe pressure. The ovaries and Fallopian tubes are often difficult to distinguish separately, with the normal tissue boundaries between the two structures becoming indiscernible, owing to purulent material, oedema and inflammation.14
Ultrasound may demonstrate a pyosalpinx as a thickened, distended tube, and a ‘cogwheel sign’ may be noted15 16 (see Figure 3). This describes the appearance of a serpinginous tubular structure filled with echogenic fluid. The cogwheel appearance is owing to prominent endosalpingeal folds. By contrast, a hydrosalpinx is filled with anechoic (in other words, simple) fluid.

Figure 3. Pyosalpinx with ‘cogwheel sign’. Transvaginal ultrasound image demonstrating two adjacent transverse sections of Fallopian tube. Note the central hypoechoic material on right with thickened endosalpingeal folds forming the cogwheel sign (A) and mixed echogenic/purulent material to the left (B).
Fibroid degeneration or torsion
Fibroids are common in reproductive age women and may occasionally cause acute pain, owing to degeneration or torsion, particularly if pedunculated. Ultrasound is the initial radiological modality of choice. Fibroids appear on imaging as well defined hypoechoic solid lesions arising from or within the myometrium. On colour Doppler, they are relatively avascular when compared to the surrounding myometrium.17
Degeneration or torsion is suggested if the pain is reproducible by probe pressure over the fibroid. Degenerating fibroids have a more complex heterogenous appearance. Anechoic or hypoechoic cystic spaces within the fibroid are suggestive of haemorrhagic/carneous and cystic degeneration.18 Calcification is also a feature.
Large fibroids rarely can cause bowel obstruction or hydronephrosis secondary to mass effect.19 The role of MRI is to further define and more accurately characterise fibroids, particularly those in difficult locations.20
Non-gynaecological causes of pelvic pain
Appendicitis
Appendicitis generally presents with right iliac fossa pain. Specific adnexal tenderness may be present if the appendix is orientated so that its tip is in the pelvis.21 Likewise, reactive pelvic or peritoneal inflammation may also cause adnexal tenderness.
On ultrasound, the appendix is variably seen. In appendicitis, it is most often seen on high-frequency linear transducer TA imaging, particularly using the graded compression technique.22 Criteria for diagnosis is a distended blind ending tubular structure >6mm in diameter (see Figure 4). There is no peristalsis and it is generally non-compressible.23 The patient is often tender to focal transducer pressure. An appendicolyth, which obstructs the lumen causing inflammation and pain, may be seen as a well-circumscribed echogenic structure with posterior acoustic shadowing (as they are often calcified).24

Figure 4. Appendicitis. Note the non-compressible, blind-ending, tubular structure measuring >6mm.
If the appendix perforates, purulent material can track into the pelvis, appearing as a complex mass separate from the ovary, although it may be difficult to delineate this on ultrasound. Transvaginal scanning to identify the ovary as separate to this inflammatory mass is beneficial.25 Soft features, if the appendix is not visualised, include echogenic intraperitoneal fat and enlarged iliocolic or mesenteric lymph nodes26.
CT is superior to ultrasound in the diagnosis of acute appendicitis with higher sensitivity and specificity.27 In patients presenting with atypical appendicitis, such as women with pelvic/lower abdominal pain, ultrasound is often the preferred modality as it is cheaper, radiation free and allows characterisation of pelvic organs.28
Diverticulitis
In an older gynaecological patient (usually >40 years) diverticulitis is another differential. These women typically present with left-sided pain. The pain may initially be experienced as pelvic pain, particularly if located in the sigmoid colon, hence referral to gynaecology.29 Simple diverticulitis is a clinical diagnosis and not seen on ultrasound. CT may demonstrate the presence of a diverticula and thickening of the sigmoid colon, with inflammatory fat stranding surrounding a diverticulum.30
Complicated diverticulitis on CT is seen as a pericolic collection, with marked surrounding inflammation and free locules of gas.31 In severe cases, surrounding structures such as the visceral peritoneum and ovaries may also become inflamed. Abscesses associated with diverticulitis may track into the pelvis and are differentiated from a TOA due to the visualisation of the ovary separate to the collection.
Mesenteric adenitis
Mesenteric adenitis is a diagnosis most commonly found in children, but may present in adolescents as right iliac fossa pain and therefore be referred initially to gynaecology. Ultrasound or CT demonstrates multiple (more than three) enlarged ileocolic lymph nodes with echogenic fat on ultrasound or fat stranding on CT. A normal appendix and absence of other pathology in the presence of nodal enlargement and pain is often diagnostic.32
Summary
This article has described the various images associated with common gynaecological and non-gynaecological causes of acute pelvic pain. Knowledge of these appearances can help the gynaecologist perform and interpret scans and, in conjunction with history, examination and laboratory testing, aid in accurate diagnosis and treatment of our population.
References
- Lambert MJ, Villa M. Gynecologic Ultrasound in Emergency Medicine. Emerg Med Clin N Am 2004;22:683-696.
- Lambert MJ, Villa M. Gynecologic Ultrasound in Emergency Medicine. Emerg Med Clin N Am 2004;22:683-696.
- Jeong YY et al. Imaging Evaluation of Ovarian Masses. RadioGraphics 2000;20:1445-1470.
- Lambert MJ, Villa M. Gynecologic Ultrasound in Emergency Medicine. Emerg Med Clin N Am 2004;22:683-696.
- Jeong YY et al. Imaging Evaluation of Ovarian Masses. RadioGraphics 2000;20:1445-1470.
- Jeong YY et al. Imaging Evaluation of Ovarian Masses. RadioGraphics 2000;20:1445-1470.
- Houry D, Abbott J. Ovarian torsion: A fifteen-year review. Annals of Emergency Medicine 2001;38:156-159.
- Albayram F, Hamper UM. Ovarian and Adnexal Torsion. J Ultrasound Med 2001;20:1083-1089.
- Albayram F, Hamper UM. Ovarian and Adnexal Torsion. J Ultrasound Med 2001;20:1083-1089.
- Albayram F, Hamper UM. Ovarian and Adnexal Torsion. J Ultrasound Med 2001;20:1083-1089.
- Albayram F, Hamper UM. Ovarian and Adnexal Torsion. J Ultrasound Med 2001;20:1083-1089.
- Lareau SM, Beigi RH, Pelvic Inflammatory Disease and Tubo-ovarian Abscess. Infect Dis Clin N Am 2008;22:693-708.
- Lareau SM, Beigi RH, Pelvic Inflammatory Disease and Tubo-ovarian Abscess. Infect Dis Clin N Am 2008;22:693-708.
- Lambert MJ, Villa M. Gynecologic Ultrasound in Emergency Medicine. Emerg Med Clin N Am 2004;22:683-696.
- Lambert MJ, Villa M. Gynecologic Ultrasound in Emergency Medicine. Emerg Med Clin N Am 2004;22:683-696.
- Lareau SM, Beigi RH, Pelvic Inflammatory Disease and Tubo-ovarian Abscess. Infect Dis Clin N Am 2008;22:693-708.
- Wilde S, Scott-Barrett S, Radiological appearances of uterine fibroids. Indian J Radiol Imaging 2009;19(3):222-231.
- Wilde S, Scott-Barrett S, Radiological appearances of uterine fibroids. Indian J Radiol Imaging 2009;19(3):222-231.
- Rao PM et al, CT diagnosis of mesenteric adenitis. Radiology 1997;202(1):145-149.
- Wilde S, Scott-Barrett S, Radiological appearances of uterine fibroids. Indian J Radiol Imaging 2009;19(3):222-231.
- Hardin M, Acute Appendicitis: Review and Update. Am Fam Physician 1999;60(7):2027-2034.
- Kessler N et al. Appendicitis: Evaluation of sensitivity, specificity and predictive values of US, Doppler US and laboratory findings. Radiology 2004;230:472-478.
- Kessler N et al. Appendicitis: Evaluation of sensitivity, specificity and predictive values of US, Doppler US and laboratory findings. Radiology 2004;230:472-478.
- Kessler N et al. Appendicitis: Evaluation of sensitivity, specificity and predictive values of US, Doppler US and laboratory findings. Radiology 2004;230:472-478.
- Kessler N et al. Appendicitis: Evaluation of sensitivity, specificity and predictive values of US, Doppler US and laboratory findings. Radiology 2004;230:472-478.
- Kessler N et al. Appendicitis: Evaluation of sensitivity, specificity and predictive values of US, Doppler US and laboratory findings. Radiology 2004;230:472-478.
- Van Randen et al, A comparison of the Accuracy of Ultrasound and Computed Tomography in common diagnoses causing acute abdominal pain. Eur Radiol. 2011; 21(7): 1535-1545.
- Lameris et al, Imaging strategies for detection of urgent conditions in patients with acute abdominal pain: diagnostic accuracy study. BMJ 2009;338:2431.
- Jacobs DO, Diverticulitis. N Engl J Med 2007;357:2057-2066
- Lameris et al, Graded compression ultrasonography and comuted tomography in acute colonic diverticulitis: Meta-analysis of test accuracy. Eur Radiol 2008;18:2498-2511.
- Lameris et al, Graded compression ultrasonography and comuted tomography in acute colonic diverticulitis: Meta-analysis of test accuracy. Eur Radiol 2008;18:2498-2511.
- Rao PM et al, CT diagnosis of mesenteric adenitis. Radiology 1997;202(1):145-149.






Leave a Reply