Congenital malformations of the female genital tract represent a group made up of a wide range of deviations from the normal anatomy.
Their true prevalence in the general population is still debated, with older studies suggesting a mean prevalence of four per cent, while newer studies including more accurate diagnostic methods indicate a mean prevalence of closer to seven per cent.
These anomalies may present in many broad fashions with the features of obstruction to menstrual flow, inability to establish sexual intercourse or reproductive failure.
These malformations arise from abnormal embryological development of one or both of the Mullerian (paramesonephric) ducts. The most well-recognised condition is the failure of the ducts to form, as in Mayer-Rokitansky-Kuster-Hauser syndrome, but there are many variations even in this condition with partial formation of the structures.
Much debate exists surrounding the classification of these malformations and we do not have, as yet, a user-friendly system that allows us to classify these entities and allow most appropriate treatment and discussion of the prognosis for these patients, particularly in terms of future fertility and reproductive outcomes. Most clinicians agree that any such system should be simple and functional, must be based in anatomy, ideally be given in one page, and allow for complete classification with the frequency of the anomalies being taken into consideration.
Case study
The following case illustrates the difficulties that can arise for diagnosis, management and future outcomes for the young patient presenting with a congenital malformation.
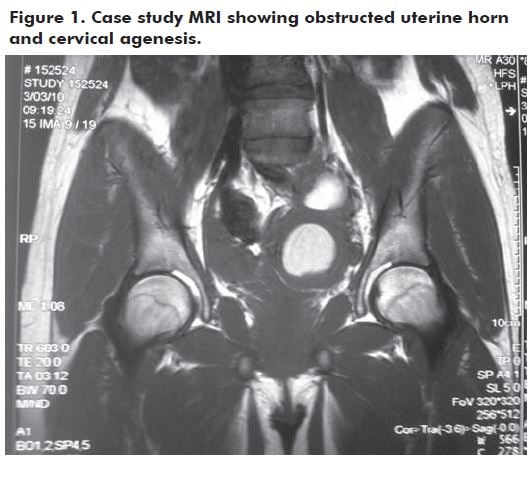
A 15-year-old girl with menarche at 13 years of age and regular cycles presented with acute lower abdominal pain. Ultrasound revealed a large pelvic mass (6 cm), thought to be a left endometrioma. Emergency laparoscopy revealed an inflammatory mass on the left side of the pelvis with the left ovary adherent to it. Filmy adhesions and intraperitoneal blood were also present. No definitive management was possible at this procedure and she was referred on to a tertiary centre. Further studies (MRI) (see Figure 1) revealed a non-communicating left uterine horn distended with blood. There was also evidence of a left haematosalpinx and a normal left ovary adherent to both structures. It was known from birth that her left kidney was absent.
She was placed on a continuous oral contraceptive pill (OCP) for two months and then definitive surgery was planned as a combined multidisciplinary procedure. Left hemi-hysterectomy and left salpingectomy using a laparoscopic approach was performed, with careful dissection and preservation of the left ovary. The cervix was clearly absent on this side and a normal right unicornuate uterus and associated structures were identified at the time of surgery.
Assessment of the renal tract and vagina was also undertaken at the time of surgery. This showed a normal right renal system, left renal agenesis and the vagina exhibited normal dimensions.
The patient has recovered well. She has been counselled regarding possible future reproductive outcomes and close obstetric surveillance has been advised.
Classification of malformations
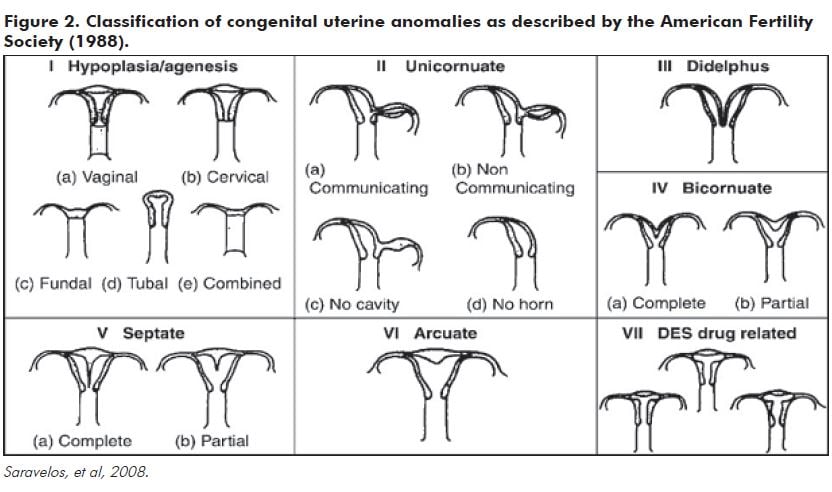
In 1988, the American Fertility Society (AFS) devised the most commonly used diagnostic classification (see Figure 2) based on the work of Buttram and Gibbons (1979). However, many anomalies are not included in the main categories, such as those disorders resulting from cervical or vaginal aplasia/dysplasia, making it incomplete and it is very difficult to categorise complex anomalies. Although other classifications have been proposed, including clinical and embryological classifications and the extensive VCuAM system (vagina, cervix, uterus, adnexae and associated malformations), these are not thought to be user-friendly and so the AFS system is still the most popular, as it is based in anatomy and seems to best correlate with pregnancy outcome.
Diagnosis and prevalence
The method used to investigate anomalies will impact on the frequency and accuracy with which the diagnosis is made. Saravelos and colleagues2 assessed the prevalence of disorders in different population groups based on their assessment of the diagnostic procedure used. They classified the diagnostic method according to diagnostic accuracy as follows.
Class 1a.
- Investigations capable of accurately identifying anomaly (greater than 90 per cent accuracy) and classifying into the appropriate subgroup.
- Hysteroscopy with laparoscopy, sonohysterogram, 3D ultrasound.
Class 1b.
- Investigations capable of identifying anomaly (greater than 90 per cent accuracy) but unable to classify into appropriate subtype.
- • Hysteroscopy alone.
Class 2.
- Investigations capable of identifying uterine anomalies with accuracy less than 90 per cent.
- Hysterosalpingogram, 2D ultrasound.
Class 3.
- Investigations in which accuracy has not been assessed – MRI.
When they assessed studies of prevalence using this classification, they found a prevalence rate in the general fertile population of 6.7 per cent if more accurate investigations were utilised compared with 2.4 per cent with Class 2 accurate methods (see Table 1).
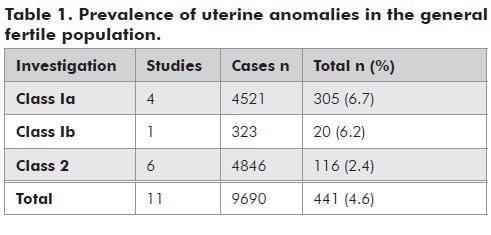
It should be noted that these studies were done in later reproductive life, so most females presenting with menstrual obstruction in adolescence or inability to have coitus are not included. Most investigations of uterine anomalies are performed in women presenting with subfertility or recurrent miscarriage. It is the author’s experience that MRI is an extremely useful diagnostic tool in the workup of the adolescent with an obstructive anomaly when planning definitive surgical management.
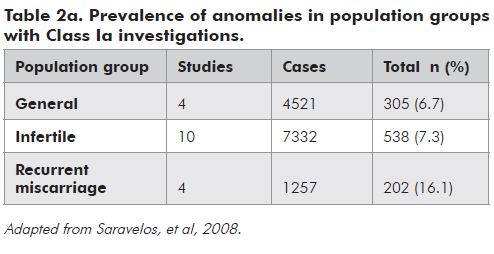
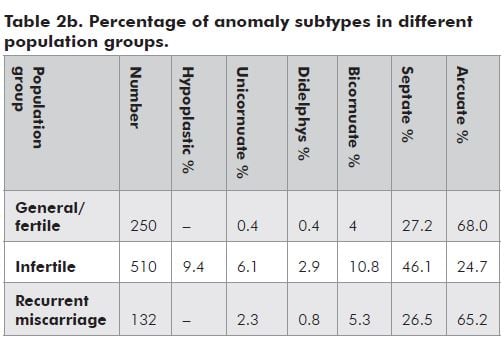
The relative prevalence in these groups when compared with the general population (using Class 1a investigations) is shown in Table 2a and 2b. This data would suggest there is an increased prevalence of anomalies in recurrent miscarriage, but not the infertile population suggesting a cause and effect in miscarriage alone. This may not be the entire truth as there is variation in the distribution of subtypes in women within different population groups.
Table 2a and 2b would suggest that hypoplastic uteri and septate uteri are more likely to be associated with infertility when Class 1a investigations are used.
Treatment
Obviously, this will depend on the presentation and stage of reproductive life the young woman is at.
For obstruction, the aim is to relieve the obstruction. This can range from a very simple release of a low vaginal septum to extremely complex surgery. The most important part is ensuring the right procedure is planned and adequate diagnosis and workup is essential. The use of continuous OCP can facilitate this and allow appropriate referral if required. It is fair to say that no two procedures are ever the same in this setting and basic sound anatomical approaches are required. The use of a combined approach with laparoscopic and vaginal operators working together is often beneficial for the best outcome.
If vaginal stenosis at any level is an issue, appropriate counselling and use of dilators can be helpful. Surgery with the input of a multidisciplinary team may also be required, particularly if previous multiple surgeries as an infant has been required, such as in infants with cloacal abnormalities.
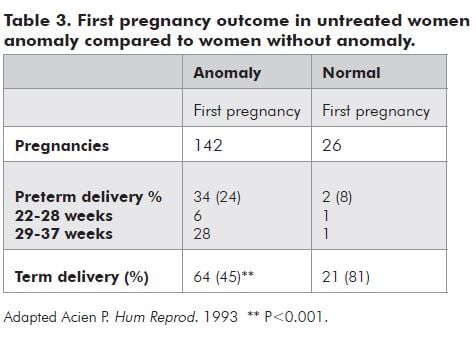
Where infertility and recurrent miscarriage are the presentation in later reproductive years, uterine anomalies are an important issue to consider, particularly in determining whether treatment is possible and likely to improve outcome. The diagnosis of a unicornuate uterus with non-communicating canulated rudimentary horn must be treated to prevent ectopic pregnancy in that horn, but other anomalies are less clear-cut. The correction and treatment of didelphic, bicornuate or unicornuate uteri is either impossible or complex and unlikely to improve the pregnancy outcome. However the advent of operative hysteroscopy using scissors, resectoscope or more recently, bipolar diathermy, in such instruments as the versapoint have meant that uterine septa can be readily divided. It is still debated whether this will improve the outcome of the pregnancy if it occurs, or improve fertility rates in the subfertile population. Acien3 (see Table 3) in small numbers suggested term delivery was significantly less likely to occur when women conceive after a diagnosis of uterine anomaly and pregnancy outcome appeared to improve after resection of the septum, although it is a less significant effect if the anomaly is arcuate or subseptate.
Conclusion
Congenital anomalies of the female genital tract represent a small but significant challenge to our practice. They may present at many ages in many guises. Appropriate assessment, diagnosis and treatment are the mainstays. Support of the individual nature of the patient’s condition needs to be acknowledged and managed. A multidisciplinary approach is appropriate for the more complex of these conditions. The true prevalence and implications for future fertility potential is yet to be determined.
References
- American Fertility Society. The AFS classification of adnexal adhesions, distal tubal occlusion, tubal occlusion secondary to tubal ligation, tubal pregnancies, Mullerian anomalies and intrauterine adhesions. Fertil Steril. 1988; 49:944-55.
- Saravelos SH, Cocksedge KA, Li T-C. Prevalence and diagnosis of congenital uterine anomalies in women with reproductive failure: a critical appraisal. Hum Reprod update 2008;14:415-29.
- Acien P. Reproductive performance of women with uterine malformations. Hum Reprod. 1993; 8:122-6.
- Grimbizis G, Campo R. Congenital malformations of the female genital tract: the need for a new classification system. Fertil Steril. 2010; 94:401-7.






Leave a Reply